Thalassemia
Topic Overview
What is thalassemia?
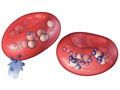
Thalassemia (say “thal-uh-SEE-mee-uh”) is an inherited blood disorder that causes your body to make less hemoglobin or abnormal hemoglobin. Hemoglobin helps red blood cells spread oxygen through your body. Low levels of hemoglobin may cause anemia, an illness that makes you feel weak and tired. Severe anemia can damage organs and lead to death.
What are the types of thalassemia?
There are two main types: alpha and beta. Beta thalassemia is the most common.
Beta thalassemia
You need both alpha- and beta-globin to make hemoglobin. Beta thalassemia occurs when one or both of the two genes that make beta-globin don’t work or only partly work as they should.
- If you have one damaged gene, you may have mild anemia and probably won’t need treatment. This is called beta thalassemia minor or beta thalassemia trait. It happens when you get a normal gene from one parent and a thalassemia gene from the other.
- When both genes are damaged, it means you got a thalassemia gene from each parent. You may have moderate or severe anemia.
- If you have moderate anemia (beta thalassemia intermedia), you may need blood transfusions.
- People with severe anemia (called beta thalassemia major or Cooley’s anemia) need blood transfusions throughout life. Symptoms of anemia usually begin within a few months after birth.
Alpha thalassemia
This type occurs when one or more of the four alpha-globin genes that make hemoglobin are missing or damaged.
- If one gene is missing or damaged: Your red blood cells might be smaller than normal. You will have no symptoms and you will not need treatment. But you are a silent carrier. This means you don’t have the disease but can pass the defective gene to your child.
- If two genes are missing or damaged: You will have very mild anemia that will typically not need treatment. This is calledalpha thalassemia minor or alpha thalassemia trait.
- If three genes are missing: You will have mild to moderately severe anemia. This is sometimes called hemoglobin H disease. If it is severe, you may need blood transfusions.
- If all four genes are missing: This is called alpha thalassemia major or hydrops fetalis. The fetus will be stillborn, or the child will die soon after birth.
What causes thalassemia?
A defect in one or more genes causes thalassemia.
If you, either parent, or any of your siblings have thalassemia or carry a gene for thalassemia and you’re thinking about having a child, you may want to talk to a genetic counselor before you get pregnant. A genetic counselor can tell you how likely it is that your child will have the disease and how severe it might be.
What are the symptoms?
Mild thalassemia usually doesn’t cause any symptoms.
Moderate or severe disease may cause symptoms of anemia. For example, you may feel weak, tire out more easily, and feel short of breath. Other symptoms also can occur depending on how severe your disease is and what problems it causes.
Children with severe thalassemia may grow slowly (failure to thrive), have skull bones that are not shaped normally, and have problems with feeding, frequent fevers, and diarrhea.
How is thalassemia diagnosed?
Your doctor will do an exam and ask about your health history. Tests you may need include:
- A complete blood count (CBC).
- A gene test to see if you have the genes that cause thalassemia.
- An iron level test.
- A blood test that measures the amounts of different types of hemoglobin, to help find out which type of thalassemia you have.
If you learn that you have thalassemia, your family members should to talk to their doctors about testing.
How is it treated?
Treatment depends on how severe your condition is.
Most large medical centers have treatment centers for blood disorders. They are an excellent resource to help you and your family get the best care.
- Mild thalassemia, the most common form, does not need treatment.
- Moderate thalassemia may be treated with blood transfusions and folic acid supplements. Folic acid is a vitamin that your body needs to produce red blood cells.
- Severe thalassemia may be treated with:
- Blood transfusions.
- Folic acid.
If you have repeated blood transfusions, it’s possible for your body to get too much iron. This can damage your heart and other organs. Make sure to avoid vitamins that contain iron, and don’t take extra vitamin C, which can increase how much iron you absorb from food. If you have too much iron, your doctor may give you chelation therapy. This is a medicine that helps remove iron from your body.
Less common treatments for severe thalassemia include:
- A blood or bone marrow stem cell transplant.
- Surgery to remove the spleen.
Get a flu vaccine each year. Also talk to your doctor about getting a pneumococcal vaccine. These vaccines may protect you from severe infections, which can make anemia worse and cause severe illness in people who have thalassemia.
References
Other Works Consulted
- Borgna-Pignatti C, Galanello R (2009). Thalassemias and related disorders: Quantitative disorders of hemoglobin synthesis. In JP Greer et al., eds., Wintrobe’s Clinical Hematology, 12th ed., vol. 1, pp. 1083–1131. Philadelphia: Lippincott Williams and Wilkins.
- Hillman R, et al. (2011). Thalassemia. In Hematology in Clinical Practice, 5th ed., pp. 65–78. New York: McGraw-Hill.
- Pennell DJ, et al. (2013). Cardiovascular function and treatment in ß-thalassemia major: A consensus statement from the American Heart Association. Circulation, 128(3): 281–308.
- Weatherall DJ (2010). The thalassemias: Disorders of globin synthesis. In K Kaushansky et al., eds., Williams Hematology, 8th ed., pp. 675–707. New York: McGraw-Hill.
Current as of: March 28, 2019
Author: Healthwise Staff
Medical Review:E. Gregory Thompson, MD – Internal Medicine & Adam Husney, MD – Family Medicine & Martin J. Gabica, MD – Family Medicine & Brian Leber, MDCM, FRCPC – Hematology
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.