Lymphedema (PDQ®): Supportive care – Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
General Information About Lymphedema
Lymphedema is the build-up of fluid in soft body tissues when the lymph system is damaged or blocked.
Lymphedema occurs when the lymph system is damaged or blocked. Fluid builds up in soft body tissues and causes swelling. It is a common problem that may be caused by cancer and cancer treatment. Lymphedema usually affects an arm or leg, but it can also affect other parts of the body. Lymphedema can cause long-term physical, psychological, and social problems for patients.
The lymph system is a network of lymph vessels, tissues, and organs that carry lymph throughout the body.
The parts of the lymph system that play a direct part in lymphedema include the following:
- Lymph: Colorless, watery fluid that travels through the lymph vessels and carries T and B lymphocytes. Lymphocytes are a type of white blood cell.
- Lymph vessels: A network of thin tubes that collect lymph from different parts of the body and return it to the bloodstream.
- Lymph nodes: Small, bean-shaped structures that filter lymph and store white blood cells that help fight infection and disease. Lymph nodes are found along a network of lymph vessels throughout the body. Groups of lymph nodes are found in the neck, underarm, mediastinum, abdomen, pelvis, and groin.
The spleen, thymus, tonsils, and bone marrow are also part of the lymph system but do not play a direct part in lymphedema.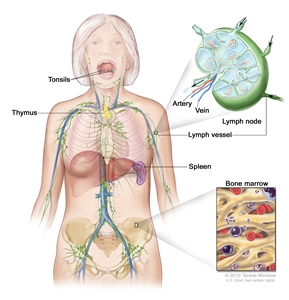
Anatomy of the lymph system showing the lymph vessels and lymph organs, including the lymph nodes, tonsils, thymus, spleen, and bone marrow. Lymph (clear fluid) and lymphocytes travel through the lymph vessels and into the lymph nodes where the lymphocytes destroy harmful substances. The lymph enters the blood through a large vein near the heart.
Lymphedema occurs when lymph is not able to flow through the body the way that it should.
When the lymph system is working as it should, lymph flows through the body and is returned to the bloodstream.
- Fluid and plasma leak out of the capillaries (smallest blood vessels) and flow around body tissues so the cells can take up nutrients and oxygen.
- Some of this fluid goes back into the bloodstream. The rest of the fluid enters the lymph system through tiny lymph vessels. These lymph vessels pick up the lymph and move it toward the heart. The lymph is slowly moved through larger and larger lymph vessels and passes through lymph nodes where waste is filtered from the lymph.
- The lymph keeps moving through the lymph system and collects near the neck, then flows into one of two large ducts:
- The right lymph duct collects lymph from the right arm and the right side of the head and chest.
- The left lymph duct collects lymph from both legs, the left arm, and the left side of the head and chest.
- These large ducts empty into veins under the collarbones, which carry the lymph to the heart, where it is returned to the bloodstream.
When part of the lymph system is damaged or blocked, fluid cannot drain from nearby body tissues. Fluid builds up in the tissues and causes swelling.
There are two types of lymphedema.
Lymphedema may be either primary or secondary:
- Primary lymphedema is caused by the abnormal development of the lymph system. Symptoms may occur at birth or later in life.
- Secondary lymphedema is caused by damage to the lymph system. The lymph system may be damaged or blocked by infection, injury, cancer, removal of lymph nodes, radiation to the affected area, or scar tissue from radiation therapy or surgery.
This summary is about secondary lymphedema in adults that is caused by cancer or cancer treatment.
Possible signs of lymphedema include swelling of the arms or legs.
Other conditions may cause the same symptoms. A doctor should be consulted if any of the following problems occur:
- Swelling of an arm or leg, which may include fingers and toes.
- A full or heavy feeling in an arm or leg.
- A tight feeling in the skin.
- Trouble moving a joint in the arm or leg.
- Thickening of the skin, with or without skin changes such as blisters or warts.
- A feeling of tightness when wearing clothing, shoes, bracelets, watches, or rings.
- Itching of the legs or toes.
- A burning feeling in the legs.
- Trouble sleeping.
- Loss of hair.
Daily activities and the ability to work or enjoy hobbies may be affected by lymphedema.
These symptoms may occur very slowly over time or more quickly if there is an infection or injury to the arm or leg.
Cancer and its treatment are risk factors for lymphedema.
Lymphedema can occur after any cancer or treatment that affects the flow of lymph through the lymph nodes, such as removal of lymph nodes. It may develop within days or many years after treatment. Most lymphedema develops within three years of surgery. Risk factors for lymphedema include the following:
- Removal and/or radiation of lymph nodes in the underarm, groin, pelvis, or neck. The risk of lymphedema increases with the number of lymph nodes affected. There is less risk with the removal of only the sentinel lymph node (the first lymph node in a group of lymph nodes to receive lymphatic drainage from the primary tumor).
- Being overweight or obese.
- Slow healing of the skin after surgery.
- A tumor that affects or blocks the left lymph duct or lymph nodes or vessels in the neck, chest, underarm, pelvis, or abdomen.
- Scar tissue in the lymph ducts under the collarbones, caused by surgery or radiation therapy.
Lymphedema often occurs in breast cancer patients who had all or part of their breast removed and axillary (underarm) lymph nodes removed. Lymphedema in the legs may occur after surgery for uterine cancer, prostate cancer, lymphoma, or melanoma. It may also occur with vulvar cancer or ovarian cancer.
Tests that examine the lymph system are used to diagnose lymphedema.
It is important to make sure there are no other causes of swelling, such as infection or blood clots. The following tests and procedures may be used to diagnose lymphedema:
- Physical exam and history: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient’s health habits and past illnesses and treatments will also be taken.
- Lymphoscintigraphy: A method used to check the lymph system for disease. A very small amount of a radioactive substance that flows through the lymph ducts and can be taken up by lymph nodes is injected into the body. A scanner or probe is used to follow the movement of this substance. Lymphoscintigraphy is used to find the sentinel lymph node (the first node to receive lymph from a tumor) or to diagnose certain diseases or conditions, such as lymphedema.
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI).
The swollen arm or leg is usually measured and compared to the other arm or leg. Measurements are taken over time to see how well treatment is working.
A grading system is also used to diagnose and describe lymphedema. Grades 1, 2, 3, and 4 are based on size of the affected limb and how severe the signs and symptoms are.
Stages may be used to describe lymphedema.
- Stage I: The limb (arm or leg) is swollen and feels heavy. Pressing on the swollen area leaves a pit (dent). This stage of lymphedema may go away without treatment.
- Stage II: The limb is swollen and feels spongy. A condition called tissue fibrosis may develop and cause the limb to feel hard. Pressing on the swollen area does not leave a pit.
- Stage III: This is the most advanced stage. The swollen limb may be very large. Stage III lymphedema rarely occurs in breast cancer patients. Stage III is also called lymphostatic elephantiasis.
Managing Lymphedema
Patients can take steps to prevent lymphedema or keep it from getting worse.
Taking preventive steps may keep lymphedema from developing. Health care providers can teach patients how to prevent and take care of lymphedema at home. If lymphedema has developed, these steps may keep it from getting worse.
Preventive steps include the following:
Tell your health care provider right away if you notice symptoms of lymphedema.
See the General Information section for symptoms that may be caused by lymphedema. Tell your doctor right away if you have any of these symptoms. The chance of improving the condition is better if treatment begins early. Untreated lymphedema can lead to problems that cannot be reversed.
Keep skin and nails clean and cared for, to prevent infection.
Bacteria can enter the body through a cut, scratch, insect bite, or other skin injury. Fluid that is trapped in body tissues by lymphedema makes it easy for bacteria to grow and cause infection. Look for signs of infection, such as redness, pain, swelling, heat, fever, or red streaks below the surface of the skin. Call your doctor right away if any of these signs appear. Careful skin and nail care helps prevent infection:
- Use cream or lotion to keep the skin moist.
- Treat small cuts or breaks in the skin with an antibacterial ointment.
- Avoid needle sticks of any type into the limb (arm or leg) with lymphedema. This includes shots or blood tests.
- Use a thimble for sewing.
- Avoid testing bath or cooking water using the limb with lymphedema. There may be less feeling (touch, temperature, pain) in the affected arm or leg, and skin might burn in water that is too hot.
- Wear gloves when gardening and cooking.
- Wear sunscreen and shoes when outdoors.
- Cut toenails straight across. See a podiatrist (foot doctor) as needed to prevent ingrown nails and infections.
- Keep feet clean and dry and wear cotton socks.
Avoid blocking the flow of fluids through the body.
It is important to keep body fluids moving, especially through an affected limb or in areas where lymphedema may develop.
- Do not cross legs while sitting.
- Change sitting position at least every 30 minutes.
- Wear only loose jewelry and clothes without tight bands or elastic.
- Do not carry handbags on the arm with lymphedema.
- Do not use a blood pressure cuff on the arm with lymphedema.
- Do not use elastic bandages or stockings with tight bands.
Keep blood from pooling in the affected limb.
- Keep the limb with lymphedema raised higher than the heart when possible.
- Do not swing the limb quickly in circles or let the limb hang down. This makes blood and fluid collect in the lower part of the arm or leg.
- Do not apply heat to the limb.
Studies have shown that carefully controlled exercise is safe for patients with lymphedema.
Exercise does not increase the chance that lymphedema will develop in patients who are at risk for lymphedema. In the past, these patients were advised to avoid exercising the affected limb. Studies have now shown that slow, carefully controlled exercise is safe and may even help keep lymphedema from developing. Studies have also shown that, in breast-cancer survivors, upper-body exercise does not increase the risk that lymphedema will develop. (See the Exercise section under Treatment of Lymphedema for more information.)
Treatment of Lymphedema
The goal of treatment is to control the swelling and other problems caused by lymphedema.
Damage to the lymph system cannot be repaired. Treatment is given to control the swelling caused by lymphedema and keep other problems from developing or getting worse. Physical (non-drug) therapies are the standard treatment. Treatment may be a combination of several of the physical methods. The goal of these treatments is to help patients continue with activities of daily living, to decrease pain, and to improve the ability to move and use the limb (arm or leg) with lymphedema. Drugs are not usually used for long-term treatment of lymphedema.
Treatment of lymphedema may include the following:
Pressure garments
Pressure garments are made of fabric that puts a controlled amount of pressure on different parts of the arm or leg to help move fluid and keep it from building up. Some patients may need to have these garments custom-made for a correct fit. Wearing a pressure garment during exercise may help prevent more swelling in an affected limb. It is important to use pressure garments during air travel, because lymphedema can become worse at high altitudes. Pressure garments are also called compression sleeves and lymphedema sleeves or stockings.
Exercise
Both light exercise and aerobic exercise (physical activity that causes the heart and lungs to work harder) help the lymph vessels move lymph out of the affected limb and decrease swelling.
- Talk with a certified lymphedema therapist before beginning exercise.
Patients who have lymphedema or who are at risk for lymphedema should talk with a certified lymphedema therapist before beginning an exercise routine. (See the Lymphology Association of North America Web site for a list of certified lymphedema therapists in the United States.)
- Wear a pressure garment if lymphedema has developed.
Patients who have lymphedema should wear a well-fitting pressure garment during all exercise that uses the affected limb or body part.
When it is not known for sure if a woman has lymphedema, upper-body exercise without a garment may be more helpful than no exercise at all. Patients who do not have lymphedema do not need to wear a pressure garment during exercise.
- Breast cancer survivors should begin with light upper-body exercise and increase it slowly.
Some studies with breast cancer survivors show that upper-body exercise is safe in women who have lymphedema or who are at risk for lymphedema. Weight-lifting that is slowly increased may keep lymphedema from getting worse. Exercise should start at a very low level, increase slowly over time, and be overseen by the lymphedema therapist. If exercise is stopped for a week or longer, it should be started again at a low level and increased slowly.
If symptoms (such as swelling or heaviness in the limb) change or increase for a week or longer, talk with the lymphedema therapist. It is likely that exercising at a low level and slowly increasing it again over time is better for the affected limb than stopping the exercise completely.
More studies are needed to find out if weight-lifting is safe for cancer survivors with lymphedema in the legs.
Bandages
Once the lymph fluid is moved out of a swollen limb, bandaging (wrapping) can help prevent the area from refilling with fluid. Bandages also increase the ability of the lymph vessels to move lymph along. Lymphedema that has not improved with other treatments is sometimes helped with bandaging.
Skin care
The goal of skin care is to prevent infection and to keep skin from drying and cracking. See skin care tips, in the Managing Lymphedema section.
Combined therapy
Combined physical therapy is a program of massage, bandaging, exercises, and skin care managed by a trained therapist. At the beginning of the program, the therapist gives many treatments over a short time to decrease most of the swelling in the limb with lymphedema. Then the patient continues the program at home to keep the swelling down. Combined therapy is also called complex decongestive therapy.
Compression device
Compression devices are pumps connected to a sleeve that wraps around the arm or leg and applies pressure on and off. The sleeve is inflated and deflated on a timed cycle. This pumping action may help move fluid through lymph vessels and veins and keep fluid from building up in the arm or leg. Compression devices may be helpful when added to combined therapy. The use of these devices should be supervised by a trained professional because too much pressure can damage lymph vessels near the surface of the skin.
Weight loss
In patients who are overweight, lymphedema related to breast cancer may improve with weight loss.
Laser therapy
Laser therapy may help decrease lymphedema swelling and skin hardness after a mastectomy. A hand-held, battery-powered device is used to aim low-level laser beams at the area with lymphedema.
Drug therapy
Lymphedema is not usually treated with drugs. Antibiotics may be used to treat and prevent infections. Other types of drugs, such as diuretics or anticoagulants (blood thinners), are usually not helpful and may make the lymphedema worse.
Surgery
Lymphedema caused by cancer is rarely treated with surgery.
Massage therapy
Massage therapy (manual therapy) for lymphedema should begin with someone specially trained in treating lymphedema. In this type of massage, the soft tissues of the body are lightly rubbed, tapped, and stroked. It is a very light touch, almost like a brushing. Massage may help move lymph out of the swollen area into an area with working lymph vessels. Patients can be taught to do this type of massage therapy themselves.
When done correctly, massage therapy does not cause medical problems. Massage should not be done on any of the following:
- Open wounds, bruises, or areas of broken skin.
- Tumors that can be seen on the skin surface.
- Areas with deep vein thrombosis (blood clot in a vein).
- Sensitive soft tissue where the skin was treated with radiation therapy.
When lymphedema is severe and does not get better with treatment, other problems may be the cause.
Sometimes severe lymphedema does not get better with treatment or it develops several years after surgery. If there is no known reason, doctors will try to find out if the problem is something other than the original cancer or cancer treatment, such as another tumor.
Lymphangiosarcoma is a rare, fast-growing cancer of the lymph vessels. It is a problem that occurs in some breast cancer patients and appears an average of 10 years after a mastectomy. Lymphangiosarcoma begins as purple lesions on the skin, which may be flat or raised. A CT scan or MRI is used to check for lymphangiosarcoma. Lymphangiosarcoma usually cannot be cured.
Current Clinical Trials
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute’s (NCI’s) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government’s center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the causes and treatment of lymphedema. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary (“Updated”) is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Supportive and Palliative Care Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become “standard.” Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI’s website. For more information, call the Cancer Information Service (CIS), NCI’s contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary].”
The best way to cite this PDQ summary is:
PDQ® Supportive and Palliative Care Editorial Board. PDQ Lymphedema. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/about-cancer/treatment/side-effects/lymphedema/lymphedema-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389292]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s E-mail Us.
Last Revised: 2019-03-07
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI’s Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.

