Top of the pageActionset
Pacemaker: Living Well With It
Introduction
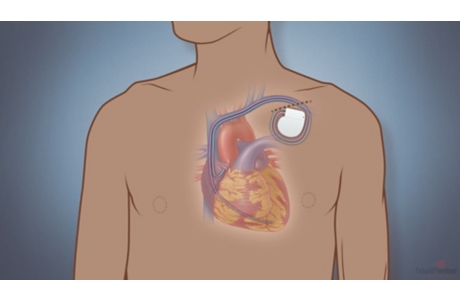
A pacemaker keeps your heart from beating too slowly. It’s important to know how this device works and how to keep it working right. Learning a few important facts about pacemakers can help you get the best results from your device.
You may have a device that combines a pacemaker and an implantable cardioverter-defibrillator (ICD), which can shock your heart back to a normal rhythm. To learn more about ICDs, see Heart Problems: Living With an ICD.
- Use certain electric devices with caution. Some electric devices have a strong electromagnetic field. This field can keep your pacemaker from working right for a short time. Check with your doctor about what you need to avoid and what you need to keep a short distance away from your pacemaker.
- Be sure that any doctor, dentist, or other health professional you see knows that you have a pacemaker.
- Always carry a card in your wallet that tells what kind of device you have. Wear medical alert jewelry that says you have a pacemaker.
- Have your pacemaker checked regularly to make sure it is working right.
How do you get the best results from a pacemaker?
Use certain electric devices with caution
Some electric devices have a strong electromagnetic field. This field can keep your pacemaker from working right for a short time. These devices are in your home, garage, workplace, and hospital.
Many other devices do not affect how a pacemaker works. You can use these safely when they are in good working condition.
Check with your doctor or the manufacturer of your pacemaker. They can give you a full list of what is safe, what you need to avoid, and what you need to keep a short distance away from your ICD.
Here are some examples.
Devices to avoid
Avoid devices with strong electromagnetic fields, such as:
- MRI machines, unless you have a device that is safe in an MRI machine or your doctor says you can safely have an MRI done with your pacemaker.
- Certain welding equipment.
- Electronic body-fat scales.
Devices to be cautious around
Keep your pacemaker at least 2 ft (0.6 m) away from:
- Induction cooktop stoves.
- Jumper cables.
- Table saws.
Keep your pacemaker at least 12 in. (30 cm) away from:
- Car battery chargers.
- Ignition systems of gasoline-powered engines or tools.
- CB radios.
Keep your pacemaker at least 6 in. (15 cm) away from:
- Cell phones and smartphones.
- Tablets and e-readers.
- Wearable devices that use wireless technology, such as fitness trackers.
- Hair dryers.
- Vacuum cleaner motors.
- Small magnets.
- Electric-powered tools such as a drill, lawn mower, or saw.
Do not stand near:
- Anti-theft detectors in stores.
- Security systems in airports.
Devices that do not affect a pacemaker
- Kitchen and bathroom equipment:
- Bathroom appliances (such as curling irons, battery-powered shavers, and electric toothbrushes)
- Kitchen appliances (such as toasters, blenders, electric can openers, and refrigerators)
- Microwave, gas, and electric ovens
- Other household items:
- Heating pads and electric blankets
- Washing machines and dryers
- Remote controls
- TVs, CD players, DVD players
- Garage door openers
- Office equipment:
- Computers
- Copy machines
- Printers
Call your doctor if an alarm goes off
Some pacemakers have an alarm system that can tell you when to call your doctor. The alarm does not mean that your pacemaker is not working. It means that your doctor needs to check something on your pacemaker. For example, an alarm might mean that the battery needs to be checked.
Your doctor can tell you what your alarm will sound like or feel like. You might hear beeping. Or you might feel a vibration, like a cell phone vibration.
Call your doctor right away if you hear or feel an alarm.
Having medical tests and procedures
Many medical tests and procedures won’t affect your pacemaker. But some procedures include electromagnetic fields that could affect how your pacemaker works. To be safe:
- Let your doctors, dentists, and other health professionals know that you have a pacemaker before you have any test, procedure, or surgery.
- Have your dentist talk to your doctor before you have any dental work or surgery.
- If you need physical therapy, have the therapist contact your doctor before using ultrasound, heat therapy, or electrical stimulation.
- If you need an MRI, check with your doctor first. An MRI can be done if you have a pacemaker that is safe for an MRI. If you have another type of pacemaker, the test might be done safely in certain cases, but you will need to talk with your doctor about the benefits and risks.
Traveling
You can travel safely with a cardiac device. But you’ll want to be prepared before you go.
- Bring a list of the names and phone numbers of your doctors.
- Bring your cardiac device identification card with you.
- Know what to do when going through airport security.
Driving
You can drive if you have a pacemaker and you don’t have any symptoms such as fainting. But right after you get a pacemaker, your doctor may ask you to not drive for at least a week after the device is implanted. This gives you time to heal.
Letting others know
- Carry a pacemaker identification card with you at all times. The card should include manufacturer information and the model number. Your doctor can give you an ID card.
- Wear medical alert jewelry stating that you have a pacemaker. You can buy this at most drugstores or online.
Having follow-up
- Go to all your appointments with your doctor to check your pacemaker. In between checkups, you will probably send information from your pacemaker to your doctor through a phone line or the Internet. You might do this manually or your device might do it automatically.
- If you take heart rhythm medicines, take them as prescribed. The medicines work with your pacemaker to help your heart keep a steady rhythm.
- Your doctor and/or the device maker will contact you about what to do if your device is recalled.
Exercising safely
Pacemakers often are used to improve your ability to exercise. Most people with pacemakers have active lives and can exercise. Talk to your doctor about the type and amount of exercise and other activity you can do.
In general:
- You may need to limit your activity if you have an irregular heart rate caused by heart failure or another heart problem.
- Talk with your doctor about what type and level of exercise is safe for you. You may choose to avoid contact sports, such as soccer or basketball, because the device can be damaged. Sports such as swimming, running, walking, tennis, golf, and bicycling are safer.
- If you want to do strength-training exercises, ask your doctor or a fitness trainer to suggest ones that are safe for someone who has a pacemaker. Some exercises might put too much strain on your device.
Having sex
Most people who have a pacemaker can have an active sex life. After you get a pacemaker implanted, you’ll let your chest heal for a short time. If your doctor says that you can exercise and be active, then it’s probably safe for you to have sex.
Talk with your doctor if you have any concerns.
Planning for the future
As you plan for your future and your end of life, you can include plans for your pacemaker. You can make the decision to turn off your pacemaker as part of the medical treatment that you want at the end of life. You can put this information in your advance directive.
When to call a doctor
Call your doctor right away if you have symptoms that could mean your device isn’t working properly, such as:
- Your heartbeat is very fast or slow, skipping, or fluttering.
- You feel dizzy, lightheaded, or faint.
- You have shortness of breath that is new or getting worse.
Call your doctor right away if you think you have an infection near your device. Signs of an infection include:
- Changes in the skin around your device, such as swelling, warmth, redness, and pain.
- An unexplained fever.
References
Other Works Consulted
- Indik JH, et al. (2017). 2017 HRS expert consensus statement on magnetic resonance imaging and radiation exposure in patients with cardiovascular implantable electronic devices. Heart Rhythm, 14(7): e97–e153. DOI: 10.1016/j.hrthm.2017.04.025. Accessed May 25, 2018.
- Baddour LM, et al. (2010). Update on cardiovascular implantable electronic device infections and their management. A scientific statement from the American Heart Association. Circulation, 121(3): 458–477.
- Lampert R, et al. (2010). HRS Expert Consensus Statement on the Management of Cardiovascular Implantable Electronic Devices (CIEDs) in patients nearing end of life or requesting withdrawal of therapy. Heart Rhythm, 7(7): 1008–1026. Available online: http://www.hrsonline.org/Policy/ClinicalGuidelines/upload/ceids_mgmt_eol.pdf.
- Lee S, et al. (2009). Clinically significant magnetic interference of implanted cardiac devices by portable headphones. Heart Rhythm, 6(10): 1432–1436.
- Levine GN, et al. (2012). Sexual activity and cardiovascular disease: A scientific statement from the American Heart Association. Circulation, 125(8): 1058–1072.
- Swerdlow CD, et al. (2015) Pacemakers and implantable cardioverter-defibrillators. In DL Mann et al., eds., Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine, 10th ed., vol. 1, pp. 721–742. Philadelphia: Saunders.
- Tjong FVY, Reddy VY (2017). Permanent leadless cardiac pacemaker therapy. Circulation, 135(15): 1458–1470. DOI: 10.1161/CIRCULATIONAHA.116.025037. Accessed March 21, 2018.
- Wilkoff BL, et al. (2008). HRS/EHRA expert consensus on the monitoring of cardiovascular implantable electronic devices (CIEDS): Description of techniques, indications, personnel, frequency, and ethical considerations. Heart Rhythm, 5(6): 907–925. Available online: http://www.hrsonline.org/Practice-Guidance/Clinical-Guidelines-Documents/HRS-EHRA-Expert-Consensus-on-the-Monitoring-of-Cardiovascular-Implantable-Electronic-Devices/2008-Monitoring-of-CIEDs.
- Zipes DP, et al. (2015). Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: Task Force 9: Arrhythmias and conduction defects: A scientific statement from the American Heart Association and American College of Cardiology. Circulation, 132(22): e315–e325. DOI: 10.1161/CIR.0000000000000245. Accessed April 7, 2017.
Credits
Current as of: April 9, 2019
Author: Healthwise Staff
Medical Review:E. Gregory Thompson MD – Internal Medicine & Martin J. Gabica MD – Family Medicine & Kathleen Romito MD – Family Medicine & Elizabeth T. Russo MD – Internal Medicine & Adam Husney MD – Family Medicine & John M. Miller MD, FACC – Cardiology, Electrophysiology
Current as of: April 9, 2019
Author: Healthwise Staff
Medical Review:E. Gregory Thompson MD – Internal Medicine & Martin J. Gabica MD – Family Medicine & Kathleen Romito MD – Family Medicine & Elizabeth T. Russo MD – Internal Medicine & Adam Husney MD – Family Medicine & John M. Miller MD, FACC – Cardiology, Electrophysiology
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.