Pacemaker for Bradycardia
Treatment Overview
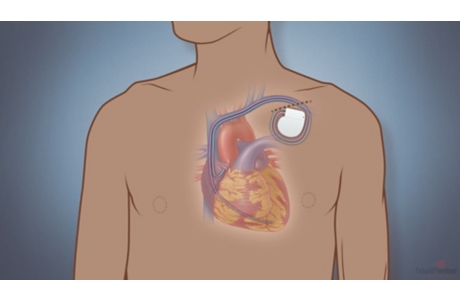
A pacemaker is a small battery-powered device that sends weak electrical impulses to “set a pace” so that the heart is able to keep a regular heartbeat.
There are different types of pacemakers, so your doctor will work with you to decide what kind will be best for you.
- Single-chamber pacemakers stimulate one chamber of the heart, either an upper chamber (atrium) or a lower one (ventricle).
- Dual-chamber pacemakers send electrical impulses to both the atrium and the ventricle and pace both chambers. A dual-chamber pacemaker synchronizes the rhythm of the atrium and ventricles in a pattern that closely resembles the natural heartbeat.
Most pacemakers are rate-responsive, or physiologic, pacemakers. This type of pacemaker varies its rate to cause the heart to beat faster when you are exercising to meet your body’s increased needs or slower when you are at rest. Another type, the fixed-rate pacemaker, sends electrical impulses at a set rate that does not vary either faster or slower. Both types of pacemakers send electrical impulses when the heart rate drops to a predetermined “slow” level.
How pacemakers are placed
Most pacemakers are surgically implanted into the chest.
The procedure to implant a pacemaker is considered minor surgery. It can usually be done using local anesthesia. Your doctor will make a small incision in your chest wall just below your collarbone. He or she then usually threads the pacemaker wires (leads) through the incision into a large blood vessel in the upper chest and into the heart. Your doctor uses X-rays to place the leads in the heart. Using the same incision, your doctor creates a small pocket under the skin to hold the pacemaker. He or she then attaches the leads to the pacemaker. The procedure takes about an hour.
Some pacemakers don’t have leads that connect to the heart. These leadless pacemakers are placed directly inside the heart.
To implant a leadless pacemaker, your doctor doesn’t need to make any cuts. Instead, he or she uses a thin tube called a catheter. The pacemaker is placed inside the catheter. The doctor puts the catheter into a blood vessel in your groin. You will get a shot to numb the skin where the catheter goes in. Then the doctor moves the catheter through the blood vessel to a lower chamber of your heart. The doctor moves the pacemaker out of the catheter. He or she attaches the pacemaker to the heart tissue. Then the catheter is removed from your body.
What To Expect
Most people stay overnight in the hospital after having a pacemaker implanted and typically go home the next day. But sometimes, the surgery is done as an outpatient procedure, which means you do not need to stay overnight in the hospital.
- If you had a pacemaker implanted under the skin of the chest, you can likely return to normal activities after a few weeks. For several weeks after the surgery, you should avoid vigorous physical activity that involves the upper body.
- If you had a leadless pacemaker implanted, your groin may have a bruise and feel sore for a day or two. You can do light activities around the house. But don’t do anything strenuous for several days.
Some electric devices have a strong electromagnetic field. This field can keep your pacemaker from working right for a short time. These devices include things in your home, garage, or workplace. Check with your doctor about what you need to avoid and what you need to keep a short distance away from your pacemaker. Many household and office electronics will not affect your pacemaker.
Your doctor will check your pacemaker regularly. Your doctor may adjust it, if needed. In between checkups at your doctor’s office, you will probably send information from your pacemaker to your doctor. You may do this by using a telephone or the Internet.
Permanent pacemakers are powered by batteries. The batteries usually last 5 to 15 years before they need to be replaced.
Why It Is Done
Your doctor might recommend that you get a pacemaker if:
- You have a problem with your heart rhythm that could be helped by a pacemaker.
- You have trouble doing everyday activities, or you can’t do them at all.
How Well It Works
Pacemakers stimulate the heart to speed up when it beats too slowly. They can also substitute for the natural pacemaker of the heart (SA node) or the heart tissue that regulates the beating of the ventricles (AV node).
Pacemakers allow people to return to normal, active lives. Most people have very few limitations, if any.
Risks
There are several risks to getting a pacemaker. But risks vary for each person. And risks vary based on the type of pacemaker you get. The chance of most problems is low.
The procedure to implant a pacemaker is safe and most people do well afterward. Afterward, you will see your doctor regularly to check your pacemaker and make sure you don’t have any problems.
During the procedure
If problems happen during the procedure, doctors can likely fix them right away. Examples include:
- A lung could collapse (pneumothorax). This happens if air builds up in the space between the lung and the chest wall. But a pneumothorax can be treated and people recover well. This problem may happen about 1 to 5 times out of a 100.footnote 1
- A tear in the heart could happen. Or a person might need emergency medicine or surgery. Based on rates of complications from patients, these problems happen about 1 time out of 100. So about 99 times out of 100, these problems do not happen.footnote 2
After the procedure
Problems after the procedure can be minor, like mild pain, or serious, like an infection. But your doctor can solve most of these problems. And most people do not have long-term issues with their pacemakers.
Problems include:
- Pain, bleeding, or bruising soon after the procedure.
- Blood clots in your arms, which cause a lot of swelling.
- Infection in your chest near the pacemaker. An infection might happen about 1 time out of 100. This means that about 99 times out of 100 there is no infection.footnote 3
- Device problems that need another procedure to fix them. For example, this might happen if a pacemaker lead breaks or a lead moves out of place.
What To Think About
In rare cases, people feel throbbing in the neck, chest fullness, or lightheadedness when the pacemaker sends out impulses. Talk to your doctor about what types of side effects you may expect from your pacemaker.
In rare cases, pacemakers are recalled by the maker of the pacemaker. A recall means that the pacemaker has a problem that needs to be watched closely or fixed.
References
Citations
- Res JCJ, et al. (2004). Pneumothorax resulting from subclavian puncture: a complication of permanent pacemaker lead implantation. Netherlands Heart Journal, 12(3): 101–105.
- Poole JE, et al. (2010). Complication rates associated with pacemaker or implantable cardioverter-defibrillator generator replacements and upgrade procedures. Circulation, 122(16): 1553–1561. DOI: 10.1161/CIRCULATIONAHA.110.976076. Accessed December 15, 2016.
- Baddour LM, et al. (2010). Update on cardiovascular implantable electronic device infections and their management. A scientific statement from the American Heart Association. Circulation, 121(3): 458–477.
Other Works Consulted
- Poole JE, et al. (2010). Complication rates associated with pacemaker or implantable cardioverter-defibrillator generator replacements and upgrade procedures. Circulation , 122(16): 1553–1561. DOI: 10.1161/CIRCULATIONAHA.110.976076. Accessed December 15, 2016.
- Swerdlow CD, et al. (2015) Pacemakers and implantable cardioverter-defibrillators. In DL Mann et al., eds., Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine, 10th ed., vol. 1, pp. 721–742. Philadelphia: Saunders.
- Tjong FVY, Reddy VY (2017). Permanent leadless cardiac pacemaker therapy. Circulation, 135(15): 1458–1470. DOI: 10.1161/CIRCULATIONAHA.116.025037. Accessed March 21, 2018.
Credits
Current as of: April 9, 2019
Author: Healthwise Staff
Medical Review:E. Gregory Thompson MD – Internal Medicine & Martin J. Gabica MD – Family Medicine & Kathleen Romito MD – Family Medicine & Adam Husney MD – Family Medicine & John M. Miller MD, FACC – Cardiology, Electrophysiology
Current as of: April 9, 2019
Author: Healthwise Staff
Medical Review:E. Gregory Thompson MD – Internal Medicine & Martin J. Gabica MD – Family Medicine & Kathleen Romito MD – Family Medicine & Adam Husney MD – Family Medicine & John M. Miller MD, FACC – Cardiology, Electrophysiology
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.