Ventricular Assist Device (VAD) for Heart Failure
Topic Overview
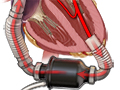
A ventricular assist device (VAD), also known as a heart pump, is a mechanical device that helps pump blood from the heart to the rest of your body.
A VAD can be implanted in the chest or worn outside the body. If it is implanted, surgery is done to place it in the chest area. The pump part of the VAD is placed in a small space in your upper abdomen. Batteries that power the pump are usually worn on a belt or pouch outside your body. After the VAD has been implanted, your doctor will make another small incision in your side to connect the electrical wires that power the device.
A VAD can help pump blood from the left side, right side, or both sides of your heart, depending on your type of heart failure.
How does it work?
A VAD helps pump blood when the heart is not able to pump enough blood on its own. It removes blood from your heart and pumps it to the rest of your body. This way, most of the blood that your heart would normally pump is pumped by the VAD instead. Most VADs have an automatic mode that adjusts to different levels of activity. For example, if you begin to walk, your VAD can increase how much blood it pumps.
Why is it used?
A VAD can be used as a temporary or long-term treatment for severe heart failure. A VAD may be used for only a short time if a person’s heart gets strong again and is able to pump blood well enough by itself. VADs may be used to help people who are waiting for a heart transplant. In some cases, VADs can be used long-term along with other heart failure treatments like medicines.
What are the benefits?
VADs used before a heart transplant can help people live until they receive the transplant.
VADs used for long-term therapy may help lower the risk of death compared to medical treatment alone. And a VAD might help a person feel better and be able to do better with daily activities.
What are the risks?
Risks from VADs include problems like stroke, excessive bleeding, infection, device malfunction, and blood clotting. These complications may need hospital care.
How do I live a normal, healthy life with a VAD?
Most people with a VAD feel better and have a better quality of life. They can be active, drive, work, be social, and enjoy hobbies.
If you have a VAD, you will have a team of specialists who will help you. They will see you regularly at follow-up visits. They will teach you how to care for your VAD at home and how to prevent problems. Self-care that you might do at home includes checking the device and changing the dressing.
How do I approach advance care planning?
Some people decide to turn off the VAD near the end of life. Making this decision can be easier after you, your doctor, and your loved ones have talked about what you can expect from your life now and in the future. When you schedule your next doctor visit, ask if you can have time to talk about your end-of-life wishes.
References
Other Works Consulted
- Aaronson KD, Pagani FD (2015). Mechanical circulatory support. In DL Mann et al., eds., Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine, 10th ed., vol. 1, pp. 590–599. Philadelphia: Saunders.
- Cook JL, et al. (2017). Recommendations for the use of mechanical circulatory support: Ambulatory and community patient care: A scientific statement from the American Heart Association. Circulation, e1145–e1158. DOI: 10.1161/CIR.0000000000000507. Accessed July 3, 2017.
- Givertz MM (2011). Ventricular assist devices: Important information for patients and families. Circulation, 124(12): e305–e311.
- Joyce D, et al. (2011). Surgical treatment of heart failure and mechanical ventricular support. In V Fuster et al., eds., Hurst’s The Heart, 13th ed., vol. 1, pp. 798–809. New York: McGraw-Hill.
- Slaughter MS, et al. (2009). Advanced heart failure treated with continuous-flow left ventricular assist device. New England Journal of Medicine, 361(23): 2241–2251.
Current as of: April 9, 2019
Author: Healthwise Staff
Medical Review:Rakesh K. Pai, MD – Cardiology, Electrophysiology & E. Gregory Thompson, MD – Internal Medicine & Martin J. Gabica, MD – Family Medicine & Adam Husney, MD – Family Medicine & David C. Stuesse, MD – Cardiac and Thoracic Surgery
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.