Laser Photocoagulation for Age-Related Macular Degeneration
Surgery Overview
The main treatment for wet age-related macular degeneration (wet AMD) is injections of medicines into the eye. But in some cases, doctors recommend laser surgery.
Retinal laser photocoagulation is a type of laser surgery that uses an intense beam of light to burn small areas of the retina. The burns form scar tissue that seals the blood vessels. By sealing the leaky blood vessels, laser photocoagulation slows down central vision loss.
Laser surgery may be done in a doctor’s office or eye clinic using a local anesthetic that affects only the eye area. The surgery itself is painless.
What To Expect
Laser photocoagulation does not involve a hospital stay. You will need someone to pick you up at the doctor’s office or clinic. Your pupils will be widened (dilated) for the surgery. And they will remain dilated for several hours. Wear sunglasses to keep bright light out of your eyes while they are dilated.
Your vision may be blurry. And your eye may hurt a little for a day or two after the surgery.
Why It Is Done
Most of the time the treatment for wet age-related macular degeneration (wet AMD) is anti-VEGF medicines that are injected into the eye. Laser treatment is not usually recommended. But for certain cases of wet AMD, laser photocoagulation may be recommended. footnote 1
How Well It Works
Laser surgery will not restore vision that has already been lost because of macular degeneration. But it can sometimes slow down or delay further damage to a person’s central vision. Even repeated treatment is not usually effective over the long term in preventing some loss of central vision.
Risks
The most serious drawback to laser surgery is that the laser damages some of the nerve cells in the macula. This causes some vision loss.
What To Think About
Your doctor will help you weigh the risks and benefits of laser surgery based on your history and the results of your exams and tests, and on his or her own experience in treating the disease.
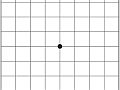
You will return for follow-up exams to make sure that the blood vessels have not started to leak again. At home, check for changes in your vision by using an Amsler grid.
Credits
Current as of: May 5, 2019
Author: Healthwise Staff
Medical Review:Kathleen Romito, MD – Family Medicine & Adam Husney, MD – Family Medicine & E. Gregory Thompson, MD – Internal Medicine & Christopher Joseph Rudnisky, MD, MPH, FRCSC – Ophthalmology
Current as of: May 5, 2019
Author: Healthwise Staff
Medical Review:Kathleen Romito, MD – Family Medicine & Adam Husney, MD – Family Medicine & E. Gregory Thompson, MD – Internal Medicine & Christopher Joseph Rudnisky, MD, MPH, FRCSC – Ophthalmology
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.