Cervical Cancer Screening (PDQ®): Screening – Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
What is screening?
Screening is looking for cancer before a person has any symptoms. This can help find cancer at an early stage. When abnormal tissue or cancer is found early, it may be easier to treat. By the time symptoms appear, cancer may have begun to spread.
Scientists are trying to better understand which people are more likely to get certain types of cancer. They also study the things we do and the things around us to see if they cause cancer. This information helps doctors recommend who should be screened for cancer, which screening tests should be used, and how often the tests should be done.
It is important to remember that your doctor does not necessarily think you have cancer if he or she suggests a screening test. Screening tests are given when you have no cancer symptoms.
If a screening test result is abnormal, you may need to have more tests done to find out if you have cancer. These are called diagnostic tests.
General Information About Cervical Cancer
Cervical cancer is a disease in which malignant (cancer) cells form in the cervix.
The cervix is the lower, narrow end of the uterus (the hollow, pear-shaped organ where a fetus grows). The cervix leads from the uterus to the vagina (birth canal).
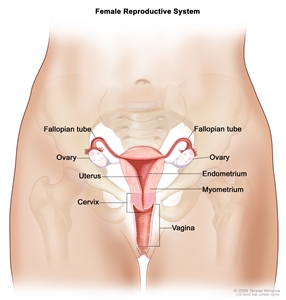
Anatomy of the female reproductive system. The organs in the female reproductive system include the uterus, ovaries, fallopian tubes, cervix, and vagina. The uterus has a muscular outer layer called the myometrium and an inner lining called the endometrium.
Cervical cancer usually develops slowly over time. Before cancer appears in the cervix, the cells of the cervix go through changes known as dysplasia, in which cells that are not normal begin to appear in the cervical tissue. Later, cancer cells start to grow and spread more deeply into the cervix and to surrounding areas.
See the following PDQ summaries for more information about cervical cancer:
- Cervical Cancer Prevention
- Cervical Cancer Treatment
Screening for cervical cancer using the Pap test has decreased the number of new cases of cervical cancer and the number of deaths due to cervical cancer since 1950.
Cervical dysplasia occurs more often in women who are in their 20s and 30s. Death from cervical cancer is rare in women younger than 30 years and in women of any age who have regular screenings with the Pap test. The Pap test is used to detect cancer and changes that may lead to cancer. The chance of death from cervical cancer increases with age. Deaths from cervical cancer occur more often in black women than in white women.
Human papillomavirus (HPV) infection is the major risk factor for cervical cancer.
Although most women with cervical cancer have the human papillomavirus (HPV) infection, not all women with an HPV infection will develop cervical cancer. Many different types of HPV can affect the cervix and only some of them cause abnormal cells that may become cancer. Some HPV infections go away without treatment.
HPV infections are spread mainly through sexual contact. Women who become sexually active at a young age and have many sexual partners are at increased risk for HPV infections.
Other risk factors for cervical cancer include:
- Giving birth to many children.
- Smoking cigarettes.
- Using oral contraceptives (“the Pill”).
- Having a weakened immune system.
Cervical Cancer Screening
Tests are used to screen for different types of cancer when a person does not have symptoms.
Scientists study screening tests to find those with the fewest harms and most benefits. Cancer screening trials also are meant to show whether early detection (finding cancer before it causes symptoms) helps a person live longer or decreases a person’s chance of dying from the disease. For some types of cancer, the chance of recovery is better if the disease is found and treated at an early stage.
Studies show that screening for cervical cancer helps decrease the number of deaths from the disease.
Regular screening of women between the ages of 21 and 65 years with the Pap test decreases their chance of dying from cervical cancer.
A Pap test is commonly used to screen for cervical cancer.
A Pap test is a procedure to collect cells from the surface of the cervix and vagina. A piece of cotton, a brush, or a small wooden stick is used to gently scrape cells from the cervix and vagina. The cells are viewed under a microscope to find out if they are abnormal. This procedure is also called a Pap smear. A new method of collecting and viewing cells has been developed, in which the cells are placed into a liquid before being placed on a slide. It is not known if the new method will work better than the standard method to reduce the number of deaths from cervical cancer.
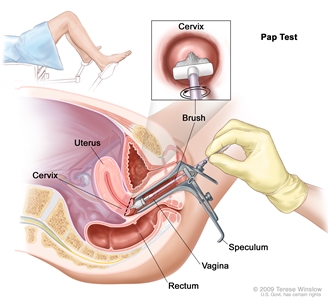
Pap test. A speculum is inserted into the vagina to widen it. Then, a brush is inserted into the vagina to collect cells from the cervix. The cells are checked under a microscope for signs of disease.
After certain positive Pap test results, an HPV test may be done.
An HPV test is a laboratory test that is used to check DNA or RNA for certain types of HPV infection. Cells are collected from the cervix and DNA or RNA from the cells is checked to find out if there is an infection caused by a type of human papillomavirus that is linked to cervical cancer. This test may be done using the sample of cells removed during a Pap test. This test may also be done if the results of a Pap test show certain abnormal cervical cells. When both the HPV test and Pap test are done using cells from the sample removed during a Pap test, it is called a Pap/HPV cotest.
An HPV test may be done with or without a Pap test to screen for cervical cancer.
Screening women aged 30 and older with both the Pap test and the HPV test every 5 years finds more cervical changes that can lead to cancer than screening with the Pap test alone. Screening with both the Pap test and the HPV test lowers the number of cases of cervical cancer.
An HPV DNA test may be used without a Pap test for cervical cancer screening in women aged 25 years and older.
Screening tests for cervical cancer are being studied in clinical trials.
Information about clinical trials supported by NCI can be found on NCI’s clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Risks of Cervical Cancer Screening
Screening tests have risks.
Decisions about screening tests can be difficult. Not all screening tests are helpful and most have risks. Before having any screening test, you may want to discuss the test with your doctor. It is important to know the risks of the test and whether it has been proven to reduce the risk of dying from cancer.
The risks of cervical cancer screening include the following:
Unnecessary follow-up tests may be done.
In women younger than 21 years, screening with the Pap test may show changes in the cells of the cervix that are not cancer. This may lead to unnecessary follow-up tests and possibly treatment. Women in this age group have a very low risk of cervical cancer and it is likely that any abnormal cells will go away on their own.
False-negative test results can occur.
Screening test results may appear to be normal even though cervical cancer is present. A woman who receives a false-negative test result (one that shows there is no cancer when there really is) may delay seeking medical care even if she has symptoms.
False-positive test results can occur.
Screening test results may appear to be abnormal even though no cancer is present. Also, some abnormal cells in the cervix never become cancer. When a Pap test shows a false-positive result (one that shows there is cancer when there really isn’t), it can cause anxiety and is usually followed by more tests and procedures (such as colposcopy, cryotherapy, or LEEP), which also have risks. The long-term effects of these procedures on fertility and pregnancy are not known.
The HPV test finds many infections that will not lead to cervical dysplasia or cervical cancer, especially in women younger than 30 years.
When both the Pap test and the HPV test are done, false-positive test results are more common.
Your doctor can advise you about your risk for cervical cancer and your need for screening tests.
Studies show that the number of cases of cervical cancer and deaths from cervical cancer are greatly reduced by screening with Pap tests. Many doctors recommend a Pap test be done every year. New studies have shown that after a woman has a Pap test and the results show no sign of abnormal cells, the Pap test can be repeated every 2 to 3 years.
The Pap test is not a helpful screening test for cervical cancer in the following groups of women:
- Women who are younger than 21 years.
- Women who have had a total hysterectomy (surgery to remove the uterus and cervix) for a condition that is not cancer.
- Women who are aged 65 years or older and have a Pap test result that shows no abnormal cells. These women are very unlikely to have abnormal Pap test results in the future.
The decision about how often to have a Pap test is best made by you and your doctor.
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute’s (NCI’s) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government’s center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about cervical cancer screening. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary (“Updated”) is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Screening and Prevention Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become “standard.” Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI’s website. For more information, call the Cancer Information Service (CIS), NCI’s contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary].”
The best way to cite this PDQ summary is:
PDQ® Screening and Prevention Editorial Board. PDQ Cervical Cancer Screening. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/cervical/patient/cervical-screening-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389215]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s E-mail Us.
Last Revised: 2019-03-08
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI’s Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.

