Childhood Non-Hodgkin Lymphoma Treatment (PDQ®): Treatment – Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
General Information About Childhood Non-Hodgkin Lymphoma
Childhood non-Hodgkin lymphoma is a disease in which malignant (cancer) cells form in the lymph system.
Childhood non-Hodgkin lymphoma is a type of cancer that forms in the lymph system, which is part of the body’s immune system. It helps protect the body from infection and disease.
The lymph system is made up of the following:
- Lymph: Colorless, watery fluid that travels through the lymph vessels and carries T and B lymphocytes. Lymphocytes are a type of white blood cell.
- Lymph vessels: A network of thin tubes that collect lymph from different parts of the body and return it to the bloodstream.
- Lymph nodes: Small, bean-shaped structures that filter lymph and store white blood cells that help fight infection and disease. Lymph nodes are found along a network of lymph vessels throughout the body. Groups of lymph nodes are found in the neck, underarm, mediastinum, abdomen, pelvis, and groin.
- Spleen: An organ that makes lymphocytes, stores red blood cells and lymphocytes, filters the blood, and destroys old blood cells. The spleen is on the left side of the abdomen near the stomach.
- Thymus: An organ in which T lymphocytes mature and multiply. The thymus is in the chest behind the breastbone.
- Tonsils: Two small masses of lymph tissue at the back of the throat. There is one tonsil on each side of the throat.
- Bone marrow: The soft, spongy tissue in the center of certain bones, such as the hip bone and breastbone. White blood cells, red blood cells, and platelets are made in the bone marrow.
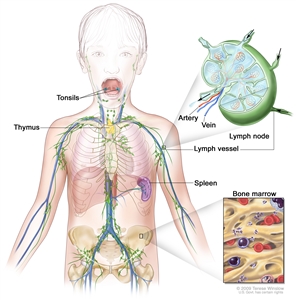
Anatomy of the lymph system, showing the lymph vessels and lymph organs including lymph nodes, tonsils, thymus, spleen, and bone marrow. Lymph (clear fluid) and lymphocytes travel through the lymph vessels and into the lymph nodes where the lymphocytes destroy harmful substances. The lymph enters the blood through a large vein near the heart.
Non-Hodgkin lymphoma can begin in B lymphocytes, T lymphocytes, or natural killer cells. Lymphocytes can also be found in the blood and collect in the lymph nodes, spleen, and thymus.
Lymph tissue is also found in other parts of the body such as the stomach, thyroid gland, brain, and skin.
Non-Hodgkin lymphoma can occur in both adults and children. Treatment for children is different than treatment for adults. See the following PDQ summaries for information about treatment of non-Hodgkin lymphoma in adults:
- Adult Non-Hodgkin Lymphoma
- Primary CNS Lymphoma Treatment
- Mycosis Fungoides (Including Sezary Syndrome) Treatment
The main types of lymphoma are Hodgkin lymphoma and non-Hodgkin lymphoma.
Lymphomas are divided into two general types: Hodgkin lymphoma and non-Hodgkin lymphoma. This summary is about the treatment of childhood non-Hodgkin lymphoma. See the PDQ summary on Childhood Hodgkin Lymphoma Treatment for information about childhood Hodgkin lymphoma.
There are three major types of childhood non-Hodgkin lymphoma.
The type of lymphoma is determined by how the cells look under a microscope. The three major types of childhood non-Hodgkin lymphoma are:
Mature B-cell non-Hodgkin lymphoma
Mature B-cell non-Hodgkin lymphomas include:
- Burkitt and Burkitt-like lymphoma/leukemia: Burkitt lymphoma and Burkitt leukemia are different forms of the same disease. Burkitt lymphoma/leukemia is an aggressive (fast-growing) disorder of B lymphocytes that is most common in children and young adults. It may form in the abdomen, Waldeyer’s ring, testicles, bone, bone marrow, skin, or central nervous system (CNS). Burkitt leukemia may start in the lymph nodes as Burkitt lymphoma and then spread to the blood and bone marrow, or it may start in the blood and bone marrow without forming in the lymph nodes first.
Both Burkitt leukemia and Burkitt lymphoma have been linked to infection with the Epstein-Barr virus (EBV), although EBV infection is more likely to occur in patients in Africa than in the United States. Burkitt and Burkitt-like lymphoma/leukemia are diagnosed when a sample of tissue is checked and a certain change to the MYCgene is found.
- Diffuse large B-cell lymphoma: Diffuse large B-cell lymphoma is the most common type of non-Hodgkin lymphoma. It is a type of B-cell non-Hodgkin lymphoma that grows quickly in the lymph nodes. The spleen, liver, bone marrow, or other organs are also often affected. Diffuse large B-cell lymphoma occurs more often in adolescents than in children.
- Primary mediastinal B-cell lymphoma: A type of lymphoma that develops from B cells in the mediastinum (the area behind the breastbone). It may spread to nearby organs including the lungs and the sac around the heart. It may also spread to lymph nodes and distant organs including the kidneys. In children and adolescents, primary mediastinal B-cell lymphoma occurs more often in older adolescents.
Lymphoblastic lymphoma
Lymphoblastic lymphoma is a type of lymphoma that mainly affects T-cell lymphocytes. It usually forms in the mediastinum (the area behind the breastbone). This causes trouble breathing, wheezing, trouble swallowing, or swelling of the head and neck. It may spread to lymph nodes, bone, bone marrow, skin, the CNS, abdominal organs, and other areas. Lymphoblastic lymphoma is a lot like acute lymphoblastic leukemia (ALL).
Anaplastic large cell lymphoma
Anaplastic large cell lymphoma is a type of lymphoma that mainly affects T-cell lymphocytes. It usually forms in the lymph nodes, skin, or bone, and sometimes forms in the gastrointestinal tract, lung, tissue that covers the lungs, and muscle. Patients with anaplastic large cell lymphoma have a receptor, called CD30, on the surface of their T cells. In many children, anaplastic large cell lymphoma is marked by changes in the ALKgene that makes a protein called anaplastic lymphoma kinase. A pathologist checks for these cell and gene changes to help diagnose anaplastic large cell lymphoma.
Some types of non-Hodgkin lymphoma are rare in children.
Some types of childhood non-Hodgkin lymphoma are less common. These include:
- Pediatric-type follicular lymphoma: In children, follicular lymphoma occurs mainly in males. It is more likely to be found in one area and does not spread to other places in the body. It usually forms in the tonsils and lymph nodes in the neck, but may also form in the testicles, kidney, gastrointestinal tract, and salivary gland.
- Marginal zone lymphoma: Marginal zone lymphoma is a type of lymphoma that tends to grow and spread slowly and is usually found at an early stage. It may be found in the lymph nodes or in areas outside the lymph nodes. Marginal zone lymphoma found outside the lymph nodes in children is called mucosa-associated lymphoid tissue (MALT) lymphoma. MALT may be linked to Helicobacter pylori infection of the gastrointestinal tract and Chlamydophila psittaci infection of the conjunctival membrane which lines the eye.
- Primary central nervous system (CNS) lymphoma: Primary CNS lymphoma is extremely rare in children.
- Peripheral T-cell lymphoma: Peripheral T-cell lymphoma is an aggressive (fast-growing) non-Hodgkin lymphoma that begins in mature T lymphocytes. The T lymphocytes mature in the thymus gland and travel to other parts of the lymph system, such as the lymph nodes, bone marrow, and spleen.
- Cutaneous T-cell lymphoma: Cutaneous T-cell lymphoma begins in the skin and can cause the skin to thicken or form a tumor. It is very rare in children, but is more common in adolescents and young adults. There are different types of cutaneous T-cell lymphoma, such as cutaneous anaplastic large cell lymphoma, subcutaneous panniculitis-like T-cell lymphoma, gamma-delta T-cell lymphoma, and mycosis fungoides. Mycosis fungoides rarely occurs in children and adolescents.
Past treatment for cancer and having a weakened immune system affect the risk of having childhood non-Hodgkin lymphoma.
Anything that increases your risk of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer; not having risk factors doesn’t mean that you will not get cancer. Talk with your child’s doctor if you think your child may be at risk.
Possible risk factors for childhood non-Hodgkin lymphoma include the following:
- Past treatment for cancer.
- Being infected with the Epstein-Barr virus or human immunodeficiency virus (HIV).
- Having a weakened immune system after a transplant or from medicines given after a transplant.
- Having certain inherited diseases (such as DNA repair defect syndromes which include ataxia-telangiectasia, Nijmegen breakage syndrome, and constitutional mismatch repair deficiency).
If lymphoma or lymphoproliferative disease is linked to a weakened immune system from certain inherited diseases, HIV infection, a transplant or medicines given after a transplant, the condition is called lymphoproliferative disease associated with immunodeficiency. The different types of lymphoproliferative disease associated with immunodeficiency include:
- Lymphoproliferative disease associated with primary immunodeficiency.
- HIV-associated non-Hodgkin lymphoma.
- Post-transplant lymphoproliferative disease.
Signs of childhood non-Hodgkin lymphoma include breathing problems and swollen lymph nodes.
These and other signs may be caused by childhood non-Hodgkin lymphoma or by other conditions. Check with a doctor if your child has any of the following:
- Trouble breathing.
- Wheezing.
- Coughing.
- High-pitched breathing sounds.
- Swelling of the head, neck, upper body, or arms.
- Trouble swallowing.
- Painless swelling of the lymph nodes in the neck, underarm, stomach, or groin.
- Painless lump or swelling in a testicle.
- Fever for no known reason.
- Weight loss for no known reason.
- Night sweats.
Tests that examine the body and lymph system are used to detect (find) and diagnose childhood non-Hodgkin lymphoma.
The following tests and procedures may be used:
- Physical exam and history: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient’s health habits and past illnesses and treatments will also be taken.
- Blood chemistry studies: A procedure in which a blood sample is checked to measure the amounts of certain substances released into the blood by organs and tissues in the body, including electrolytes, lactate dehydrogenase (LDH), uric acid, blood urea nitrogen (BUN), creatinine, and liver function values. An unusual (higher or lower than normal) amount of a substance can be a sign of disease.
- Liver function tests: A procedure in which a blood sample is checked to measure the amounts of certain substances released into the blood by the liver. A higher than normal amount of a substance can be a sign of cancer.
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
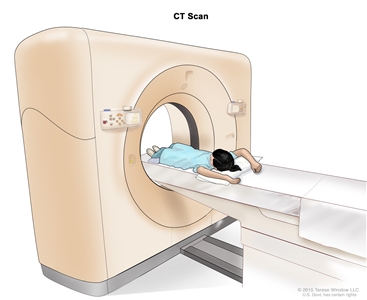
Computed tomography (CT) scan of the abdomen. The child lies on a table that slides through the CT scanner, which takes x-ray pictures of the inside of the abdomen. - PET scan (positron emission tomography scan): A procedure to find malignant tumor cells in the body. A small amount of radioactive glucose (sugar) is injected into a vein. The PET scanner rotates around the body and makes a picture of where glucose is being used in the body. Malignant tumor cells show up brighter in the picture because they are more active and take up more glucose than normal cells do. Sometimes a PET scan and a CT scan are done at the same time. If there is any cancer, this increases the chance that it will be found.
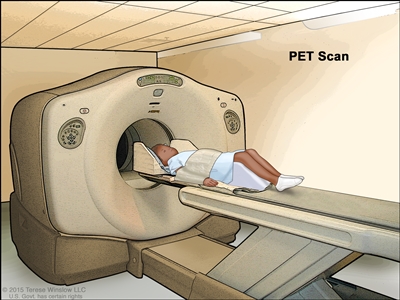
Positron emission tomography (PET) scan. The child lies on a table that slides through the PET scanner. The head rest and white strap help the child lie still. A small amount of radioactive glucose (sugar) is injected into the child’s vein, and a scanner makes a picture of where the glucose is being used in the body. Cancer cells show up brighter in the picture because they take up more glucose than normal cells do. - MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI).
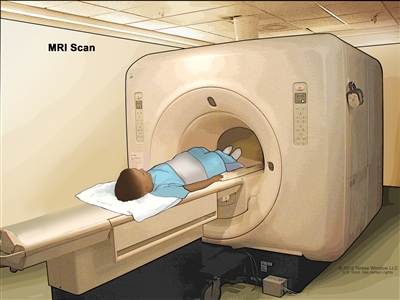
Magnetic resonance imaging (MRI) of the abdomen. The child lies on a table that slides into the MRI scanner, which takes pictures of the inside of the body. The pad on the child’s abdomen helps make the pictures clearer. - Lumbar puncture: A procedure used to collect cerebrospinal fluid (CSF) from the spinal column. This is done by placing a needle between two bones in the spine and into the CSF around the spinal cord and removing a sample of the fluid. The sample of CSF is checked under a microscope for signs that the cancer has spread to the brain and spinal cord. This procedure is also called an LP or spinal tap.
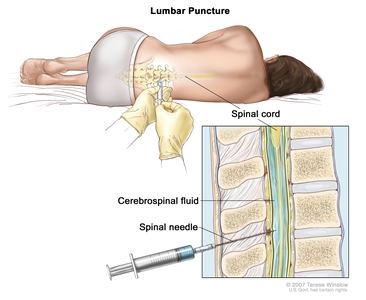
Lumbar puncture. A patient lies in a curled position on a table. After a small area on the lower back is numbed, a spinal needle (a long, thin needle) is inserted into the lower part of the spinal column to remove cerebrospinal fluid (CSF, shown in blue). The fluid may be sent to a laboratory for testing. - Chest x-ray: An x-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.
- Ultrasound exam: A procedure in which high-energy sound waves (ultrasound) are bounced off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram. The picture can be printed to be looked at later.
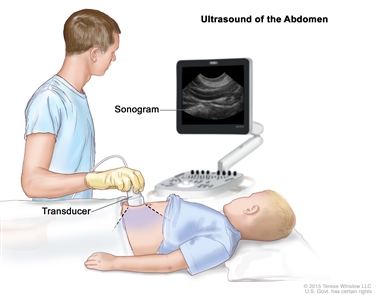
Abdominal ultrasound. An ultrasound transducer connected to a computer is pressed against the skin of the abdomen. The transducer bounces sound waves off internal organs and tissues to make echoes that form a sonogram (computer picture).
A biopsy is done to diagnose childhood non-Hodgkin lymphoma.
Cells and tissues are removed during a biopsy so they can be viewed under a microscope by a pathologist to check for signs of cancer. Because treatment depends on the type of non-Hodgkin lymphoma, biopsy samples should be checked by a pathologist who has experience in diagnosing childhood non-Hodgkin lymphoma.
One of the following types of biopsies may be done:
- Excisional biopsy: The removal of an entire lymph node or lump of tissue.
- Incisional biopsy: The removal of part of a lump, lymph node, or sample of tissue.
- Core biopsy: The removal of tissue or part of a lymph node using a wide needle.
- Fine-needle aspiration (FNA) biopsy: The removal of tissue or part of a lymph node using a thin needle.
The procedure used to remove the sample of tissue depends on where the tumor is in the body:
- Bone marrow aspiration and biopsy: The removal of bone marrow and a small piece of bone by inserting a hollow needle into the hipbone or breastbone.
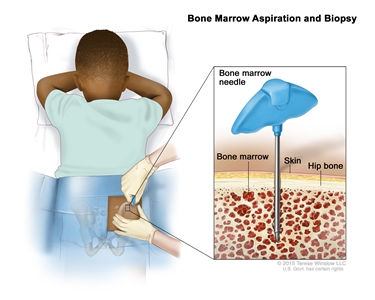
Bone marrow aspiration and biopsy. After a small area of skin is numbed, a bone marrow needle is inserted into the child’s hip bone. Samples of blood, bone, and bone marrow are removed for examination under a microscope. - Mediastinoscopy: A surgical procedure to look at the organs, tissues, and lymph nodes between the lungs for abnormal areas. An incision (cut) is made at the top of the breastbone and a mediastinoscope is inserted into the chest. A mediastinoscope is a thin, tube-like instrument with a light and a lens for viewing. It also has a tool to remove tissue or lymph node samples, which are checked under a microscope for signs of cancer.
- Anterior mediastinotomy: A surgical procedure to look at the organs and tissues between the lungs and between the breastbone and heart for abnormal areas. An incision (cut) is made next to the breastbone and a mediastinoscope is inserted into the chest. A mediastinoscope is a thin, tube-like instrument with a light and a lens for viewing. It also has a tool to remove tissue or lymph node samples, which are checked under a microscope for signs of cancer. This is also called the Chamberlain procedure.
- Thoracentesis: The removal of fluid from the space between the lining of the chest and the lung, using a needle. A pathologist views the fluid under a microscope to look for cancer cells.
If cancer is found, the following tests may be done to study the cancer cells:
- Immunohistochemistry: A laboratory test that uses antibodies to check for certain antigens in a sample of tissue. The antibody is usually linked to a radioactive substance or a dye that causes the tissue to light up under a microscope. This type of test may be used to tell the difference between different types of cancer.
- Flow cytometry: A laboratory test that measures the number of cells in a sample, the percentage of live cells in a sample, and certain characteristics of cells, such as size, shape, and the presence of tumor markers on the cell surface. The cells are stained with a light-sensitive dye, placed in a fluid, and passed in a stream before a laser or other type of light. The measurements are based on how the light-sensitive dye reacts to the light.
- Cytogenetic analysis: A laboratory test in which cells in a sample of tissue are viewed under a microscope to look for certain changes in the chromosomes.
- FISH (fluorescence in situ hybridization): A laboratory test used to look at genes or chromosomes in cells and tissues. Pieces of DNA that contain a fluorescent dye are made in the laboratory and added to cells or tissues on a glass slide. When these pieces of DNA attach to certain genes or areas of chromosomes on the slide, they light up when viewed under a microscope with a special light. This type of test is used to find certain gene changes.
- Immunophenotyping: A laboratory test used to identify cells, based on the types of antigens or markers on the surface of the cell. This test is used to diagnose specific types of lymphoma by comparing the cancer cells to normal cells of the immune system.
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis (chance of recovery) and treatment options depend on:
- The type of lymphoma.
- Where the tumor is in the body when the tumor is diagnosed.
- The stage of the cancer.
- Whether there are certain changes in the chromosomes.
- The type of initial treatment.
- Whether the lymphoma responded to initial treatment.
- The patient’s age and general health.
Stages of Childhood Non-Hodgkin Lymphoma
After childhood non-Hodgkin lymphoma has been diagnosed, tests are done to find out if cancer cells have spread within the lymph system or to other parts of the body.
The process used to find out if cancer has spread within the lymph system or to other parts of the body is called staging. The results of tests and procedures used to diagnose non-Hodgkin lymphoma may also be used for staging. See the General Information section for a description of these tests and procedures. The information gathered from the staging process determines the stage of the disease. It is important to know the stage in order to plan treatment.
The following procedure also may be used to determine the stage:
- Bone scan: A procedure to check if there are rapidly dividing cells, such as cancer cells, in the bone. A very small amount of radioactive material is injected into a vein and travels through the bloodstream. The radioactive material collects in the bones with cancer and is detected by a scanner.
There are three ways that cancer spreads in the body.
Cancer can spread through tissue, the lymph system, and the blood:
- Tissue. The cancer spreads from where it began by growing into nearby areas.
- Lymph system. The cancer spreads from where it began by getting into the lymph system. The cancer travels through the lymph vessels to other parts of the body.
- Blood. The cancer spreads from where it began by getting into the blood. The cancer travels through the blood vessels to other parts of the body.
The following stages are used for childhood non-Hodgkin lymphoma:
Stage I
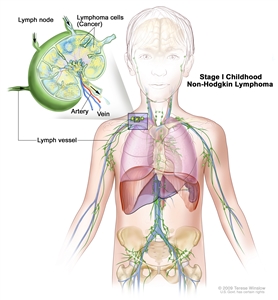
Stage I childhood non-Hodgkin lymphoma. Cancer is found in one group of lymph nodes or one area outside the lymph nodes, but no cancer is found in the abdomen or mediastinum (area between the lungs).
In stage I childhood non-Hodgkin lymphoma, cancer is found:
- in one group of lymph nodes; or
- in one area outside the lymph nodes.
No cancer is found in the abdomen or mediastinum (area between the lungs).
Stage II
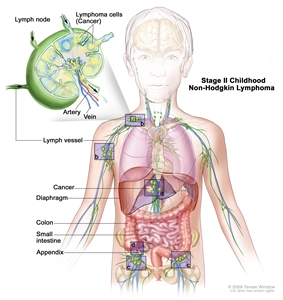
Stage II childhood non-Hodgkin lymphoma. Cancer is found in one area outside the lymph nodes and in nearby lymph nodes (a); or in two or more areas above (b) or below (c) the diaphragm; or cancer started in the stomach, appendix, or intestines (d) and can be removed by surgery.
In stage II childhood non-Hodgkin lymphoma, cancer is found:
- in one area outside the lymph nodes and in nearby lymph nodes; or
- in two or more areas either above or below the diaphragm, and may have spread to nearby lymph nodes; or
- to have started in the stomach or intestines and can be completely removed by surgery. Cancer may have spread to certain nearby lymph nodes.
Stage III
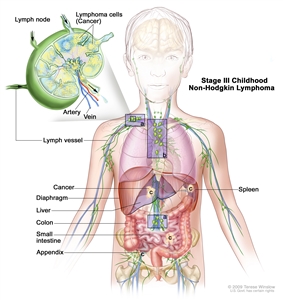
Stage III childhood non-Hodgkin lymphoma. Cancer is found in at least one area above and below the diaphragm (a); or cancer started in the chest (b); or cancer started in the abdomen and spread throughout the abdomen (c); or in the area around the spine (not shown).
In stage III childhood non-Hodgkin lymphoma, cancer is found:
- in at least one area above the diaphragm and in at least one area below the diaphragm; or
- to have started in the chest; or
- to have started in the abdomen and spread throughout the abdomen; or
- in the area around the spine.
Stage IV
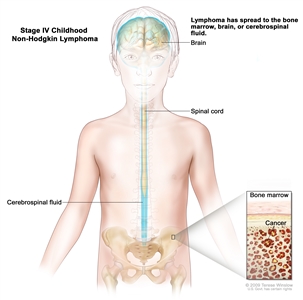
Stage IV childhood non-Hodgkin lymphoma. Cancer is found in the bone marrow, brain, or cerebrospinal fluid (CSF). Cancer may also be found in other parts of the body.
In stage IV childhood non-Hodgkin lymphoma, cancer is found in the bone marrow, brain, or cerebrospinal fluid. Cancer may also be found in other parts of the body.
Recurrent Childhood Non-Hodgkin Lymphoma
Recurrent childhood non-Hodgkin lymphoma is cancer that has recurred (come back) after it has been treated. Childhood non-Hodgkin lymphoma may come back in the lymph system or in other parts of the body.
Treatment Option Overview
There are different types of treatment for children with non-Hodgkin lymphoma.
Different types of treatment are available for children with non-Hodgkin lymphoma. Some treatments are standard (the currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment.
Taking part in a clinical trial should be considered for all children with non-Hodgkin lymphoma. Some clinical trials are open only to patients who have not started treatment.
Children with non-Hodgkin lymphoma should have their treatment planned by a team of doctors who are experts in treating childhood cancer.
Treatment will be overseen by a pediatric oncologist, a doctor who specializes in treating children with cancer. The pediatric oncologist works with other health care providers who are experts in treating children with non-Hodgkin lymphoma and who specialize in certain areas of medicine. These may include the following specialists:
- Pediatrician.
- Radiation oncologist.
- Pediatric hematologist.
- Pediatric surgeon.
- Pediatric nurse specialist.
- Rehabilitation specialist.
- Psychologist.
- Social worker.
Treatment for childhood non-Hodgkin lymphoma may cause side effects.
For information about side effects that begin during treatment for cancer, see our Side Effects page.
Side effects from cancer treatment that begin after treatment and continue for months or years are called late effects. Late effects of cancer treatment may include the following:
- Physical problems.
- Changes in mood, feelings, thinking, learning, or memory.
- Second cancers (new types of cancer).
Some late effects may be treated or controlled. It is important to talk with your child’s doctors about the effects cancer treatment can have on your child. (See the PDQ summary on Late Effects of Treatment for Childhood Cancer for more information.)
Six types of standard treatment are used:
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly into the cerebrospinal fluid (intrathecal chemotherapy), an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas. Combination chemotherapy is treatment using two or more anticancer drugs.
The way the chemotherapy is given depends on the type and stage of the cancer being treated.
Intrathecal chemotherapy may be used to treat childhood non-Hodgkin lymphoma that has spread, or may spread, to the brain. When used to lessen the chance cancer will spread to the brain, it is called CNS prophylaxis. Intrathecal chemotherapy is given in addition to chemotherapy by mouth or vein. Higher than usual doses of chemotherapy may also be used as CNS prophylaxis.
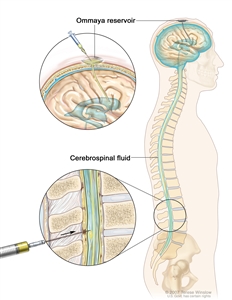
Intrathecal chemotherapy. Anticancer drugs are injected into the intrathecal space, which is the space that holds the cerebrospinal fluid (CSF, shown in blue). There are two different ways to do this. One way, shown in the top part of the figure, is to inject the drugs into an Ommaya reservoir (a dome-shaped container that is placed under the scalp during surgery; it holds the drugs as they flow through a small tube into the brain). The other way, shown in the bottom part of the figure, is to inject the drugs directly into the CSF in the lower part of the spinal column, after a small area on the lower back is numbed.
See Drugs Approved for Non-Hodgkin Lymphoma for more information.
Radiation therapy
Radiation therapy is a cancer treatment that uses high energy x-rays or other types of radiation to kill cancer cells or keep them from growing. There are two types of radiation therapy:
- External radiation therapy uses a machine outside the body to send radiation toward the cancer.
- Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer.
The way the radiation therapy is given depends on the type of non-Hodgkin lymphoma being treated. External radiation therapy may be used to treat childhood non-Hodgkin lymphoma that has spread, or may spread, to the brain and spinal cord. Internal radiation therapy is not used to treat non-Hodgkin lymphoma.
High-dose chemotherapy with stem cell transplant
High doses of chemotherapy are given to kill cancer cells. Healthy cells, including blood -forming cells, are also destroyed by the cancer treatment. Stem cell transplant is a treatment to replace the blood-forming cells. Stem cells (immature blood cells) are removed from the blood or bone marrow of the patient or a donor and are frozen and stored. After the patient completes chemotherapy, the stored stem cells are thawed and given back to the patient through an infusion. These reinfused stem cells grow into (and restore) the body’s blood cells.
See Drugs Approved for Non-Hodgkin Lymphoma for more information.
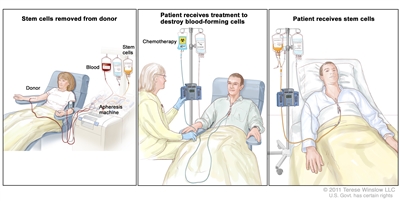
Stem cell transplant. (Step 1): Blood is taken from a vein in the arm of the donor. The patient or another person may be the donor. The blood flows through a machine that removes the stem cells. Then the blood is returned to the donor through a vein in the other arm. (Step 2): The patient receives chemotherapy to kill blood-forming cells. The patient may receive radiation therapy (not shown). (Step 3): The patient receives stem cells through a catheter placed into a blood vessel in the chest.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells without harming normal cells. Monoclonal antibodies, tyrosine kinase inhibitors, and immunotoxins are three types of targeted therapy being used or studied in the treatment of childhood non-Hodgkin lymphoma.
Monoclonal antibody therapy is a cancer treatment that uses antibodies made in the laboratory from a single type of immune system cell. These antibodies can identify substances on cancer cells or normal substances that may help cancer cells grow. The antibodies attach to the substances and kill the cancer cells, block their growth, or keep them from spreading. Monoclonal antibodies are given by infusion. They may be used alone or to carry drugs, toxins, or radioactive material directly to cancer cells.
- Rituximab is used to treat several types of childhood non-Hodgkin lymphoma.
- Pembrolizumab is used to treat primary mediastinal large B-cell lymphoma that has not responded to treatment or has recurred (come back) after treatment with other therapy. Treatment with pembrolizumab has been mostly studied in adults.
- Brentuximab vedotin is a monoclonal antibody combined with an anticancer drug that is used to treat anaplastic large cell lymphoma.
A bispecific monoclonal antibody is made up of two different monoclonal antibodies that bind to two different substances and kills cancer cells. Bispecific monoclonal antibody therapy is used in the treatment of Burkitt and Burkitt-like lymphoma /leukemia and diffuse large B-cell lymphoma.
Tyrosine kinase inhibitors (TKIs) block signals that tumors need to grow. Some TKIs also keep tumors from growing by preventing the growth of new blood vessels to the tumors. Other types of kinase inhibitors, such as crizotinib, are being studied for childhood non-Hodgkin lymphoma.
Immunotoxins can bind to cancer cells and kill them. Denileukin diftitox is an immunotoxin used to treat cutaneous T-cell lymphoma.
Targeted therapy is being studied for the treatment of childhood non-Hodgkin lymphoma that has recurred (come back).
See Drugs Approved for Non-Hodgkin Lymphoma for more information.
Other drug therapy
Retinoids are drugs related to vitamin A. Retinoid therapy with bexarotene is used to treat several types of cutaneous T-cell lymphoma.
Steroids are hormones made naturally in the body. They can also be made in a laboratory and used as drugs. Steroid therapy is used to treat cutaneous T-cell lymphoma.
Phototherapy
Phototherapy is a cancer treatment that uses a drug and a certain type of laser light to kill cancer cells. A drug that is not active until it is exposed to light is injected into a vein. The drug collects more in cancer cells than in normal cells. For skin cancer in the skin, laser light is shined onto the skin and the drug becomes active and kills the cancer cells. Phototherapy is used in the treatment of cutaneous T-cell lymphoma.
New types of treatment are being tested in clinical trials.
This summary section describes treatments that are being studied in clinical trials. It may not mention every new treatment being studied. Information about clinical trials is available from the NCI website.
Immunotherapy
Immunotherapy is a treatment that uses the patient’s immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body’s natural defenses against cancer. This type of cancer treatment is also called biotherapy or biologic therapy.
Epstein-Barr virus (EBV)-specific cytotoxic T-lymphocytes are a type of immune cell that can kill certain cells, including foreign cells, cancer cells, and cells infected with the EBV. Cytotoxic T-lymphocytes can be separated from other blood cells, grown in the laboratory, and then given to the patient to kill cancer cells. EBV-specific cytotoxic T-lymphocytes are being studied to treat post-transplant lymphoproliferative disease.
Patients may want to think about taking part in a clinical trial.
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Many of today’s standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Patients can enter clinical trials before, during, or after starting their cancer treatment.
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from recurring (coming back) or reduce the side effects of cancer treatment.
Clinical trials are taking place in many parts of the country. Information about clinical trials supported by NCI can be found on NCI’s clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Follow-up tests may be needed.
Some of the tests that were done to diagnose the cancer or to find out the stage of the cancer may be repeated. Some tests will be repeated in order to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your child’s condition has changed or if the cancer has recurred (come back). These tests are sometimes called follow-up tests or check-ups.
Treatment Options for Childhood Non-Hodgkin Lymphoma
For information about the treatments listed below, see the Treatment Option Overview section.
Burkitt and Burkitt-like lymphoma/leukemia
Treatment options for newly diagnosed Burkitt and Burkitt-like lymphoma/leukemia
Treatment options for newly diagnosed Burkitt and Burkitt-like lymphoma /leukemia may include:
- Surgery to remove as much of the tumor as possible, followed by combination chemotherapy.
- Combination chemotherapy with or without targeted therapy (rituximab).
Treatment options for recurrent Burkitt and Burkitt-like lymphoma/leukemia
Treatment options for recurrent Burkitt and Burkitt-like non-Hodgkin lymphoma /leukemia may include:
- Combination chemotherapy with or without targeted therapy (rituximab).
- High-dose chemotherapy with stem cell transplant with the patient’s own cells or cells from a donor.
- Targeted therapy with a bispecific antibody.
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Diffuse large B-cell lymphoma
Treatment options for newly diagnosed diffuse large B-cell lymphoma
Treatment options for newly diagnosed diffuse large B-cell lymphoma may include:
- Surgery to remove as much of the tumor as possible, followed by combination chemotherapy.
- Combination chemotherapy with or without targeted therapy (rituximab).
Treatment options for recurrent diffuse large B-cell lymphoma
Treatment options for recurrent diffuse large B-cell lymphoma may include:
- Combination chemotherapy with or without targeted therapy (rituximab).
- High-dose chemotherapy with stem cell transplant with the patient’s own cells or cells from a donor.
- Targeted therapy with a bispecific antibody.
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Primary Mediastinal B-cell Lymphoma
Treatment options for newly diagnosed primary mediastinal B-cell lymphoma
Treatment options for newly diagnosed primary mediastinal B-cell lymphoma may include:
- Combination chemotherapy and targeted therapy (rituximab).
Treatment options for recurrent primary mediastinal B-cell lymphoma
Treatment options for recurrent primary mediastinal B-cell lymphoma may include:
- Targeted therapy (pembrolizumab).
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Lymphoblastic Lymphoma
Treatment options for newly diagnosed lymphoblastic lymphoma
Lymphoblastic lymphoma may be classified as the same disease as acute lymphoblastic leukemia (ALL). Treatment options for lymphoblastic lymphoma may include:
- Combination chemotherapy. CNS prophylaxis with radiation therapy may also be given if cancer has spread to the brain or spinal cord.
- A clinical trial of chemotherapy with different regimens for CNS prophylaxis.
- A clinical trial of combination chemotherapy with or without targeted therapy (bortezomib).
Treatment options for recurrent lymphoblastic lymphoma
Treatment options for recurrent lymphoblastic lymphoma may include:
- Chemotherapy.
- High-dose chemotherapy with stem cell transplant with cells from a donor.
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Anaplastic Large Cell Lymphoma
Treatment options for newly diagnosed anaplastic large cell lymphoma
Treatment options for anaplastic large cell lymphoma may include:
- Surgery followed by combination chemotherapy.
- Combination chemotherapy.
- Intrathecal and systemic chemotherapy, for patients with cancer in the brain or spinal cord.
- A clinical trial of targeted therapy (crizotinib or brentuximab) and combination chemotherapy.
Treatment options for recurrent anaplastic large cell lymphoma
Treatment options for recurrent anaplastic large cell lymphoma may include:
- Chemotherapy, brentuximab, and/or crizotinib.
- Stem cell transplant with the patient’s own cells or cells from a donor.
- A clinical trial of targeted therapy (crizotinib or brentuximab) and combination chemotherapy.
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Lymphoproliferative Disease Associated With Immunodeficiency in Children
Treatment options for lymphoproliferative disease associated with primary immunodeficiency
Treatment options for lymphoproliferative disease in children and adolescents with weakened immune systems may include:
- Chemotherapy with or without rituximab.
- Stem cell transplant with cells from a donor.
Treatment options for non-Hodgkin lymphoma associated with DNA repair defect syndromes
Treatment options for non-Hodgkin lymphoma associated with DNA repair defect syndromes in children may include:
- Chemotherapy.
Treatment options for HIV-associated non-Hodgkin lymphoma
Treatment with highly active antiretroviral therapy or HAART (a combination of antiretroviral drugs) lowers the risk of non-Hodgkin lymphoma in patients infected with the human immunodeficiency virus (HIV).
Treatment options for HIV-related non-Hodgkin lymphoma (NHL) in children may include:
- Chemotherapy with or without rituximab.
For treatment of recurrent disease, treatment options depend on the type of non-Hodgkin lymphoma.
Treatment options for post-transplant lymphoproliferative disease
Treatment options for post-transplant lymphoproliferative disease may include:
- Surgery to remove the tumor. If possible, lower doses of immunosuppressive drugs after a stem cell or organ transplant may be given.
- Targeted therapy (rituximab).
- Chemotherapy with or without targeted therapy (rituximab).
- A treatment of immunotherapy using donor lymphocytes or the patient’s own T cells to target Epstein-Barr infection is being studied. This treatment is only available at a few centers in the United States.
Rare NHL Occurring in Children
Treatment options for pediatric-type follicular lymphoma
Treatment options for follicular lymphoma in children may include:
- Surgery.
- Combination chemotherapy with or without rituximab.
For children whose cancer has certain changes in the genes, treatment is similar to that given to adults with follicular lymphoma. See the Follicular Lymphoma section in the PDQ summary on Adult Non-Hodgkin Lymphoma for information.
Treatment options for marginal zone lymphoma
Treatment options for marginal zone lymphoma (including mucosa-associated lymphoid tissue (MALT) lymphoma) in children may include:
- Surgery.
- Radiation therapy.
- Rituximab with or without chemotherapy.
- Antibiotic therapy, for MALT lymphoma.
Treatment options for primary CNS lymphoma
Treatment options for primary CNS lymphoma in children may include:
- Chemotherapy.
Treatment options for peripheral T-cell lymphoma
Treatment options for peripheral T-cell lymphoma in children may include:
- Chemotherapy.
- Radiation therapy.
- Stem cell transplant with the patient’s own cells or cells from a donor.
Treatment options for cutaneous T-cell lymphoma
Treatment options for subcutaneous panniculitis-like cutaneous T-cell lymphoma in children may include:
- Watchful waiting.
- High-dose steroids.
- Targeted therapy (denileukin diftitox).
- Combination chemotherapy.
- Retinoid therapy.
- Stem cell transplant.
Treatment options for cutaneous anaplastic large cell lymphoma may include:
- Surgery, radiation therapy, or both.
In children, treatment options for mycosis fungoides may include:
- Steroids applied to the skin.
- Retinoid therapy.
- Radiation therapy.
- Phototherapy (light therapy using ultraviolet B radiation).
To Learn More About Childhood Non-Hodgkin Lymphoma
For more information from the National Cancer Institute about childhood non-Hodgkin lymphoma, see the following:
- Computed Tomography (CT) Scans and Cancer
- Drugs Approved for Non-Hodgkin Lymphoma
- Blood-Forming Stem Cell Transplants
- Targeted Cancer Therapies
For more childhood cancer information and other general cancer resources, see the following:
- About Cancer
- Childhood Cancers
- CureSearch for Children’s Cancer
- Late Effects of Treatment for Childhood Cancer
- Adolescents and Young Adults with Cancer
- Children with Cancer: A Guide for Parents
- Cancer in Children and Adolescents
- Staging
- Coping with Cancer
- Questions to Ask Your Doctor about Cancer
- For Survivors and Caregivers
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute’s (NCI’s) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government’s center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the treatment of childhood non-Hodgkin lymphoma. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary (“Updated”) is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Pediatric Treatment Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become “standard.” Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI’s website. For more information, call the Cancer Information Service (CIS), NCI’s contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary].”
The best way to cite this PDQ summary is:
PDQ® Pediatric Treatment Editorial Board. PDQ Childhood Non-Hodgkin Lymphoma Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/lymphoma/patient/child-nhl-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389294]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s E-mail Us.
Last Revised: 2019-05-24
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI’s Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.
Topic Contents
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.

