Top of the pageActionset
Diabetes: Counting Carbs if You Use Insulin
Introduction
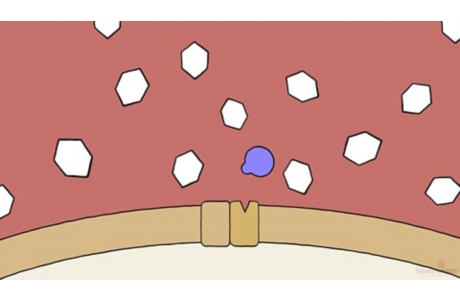
Carbohydrate, or carb, counting is an important skill to learn when you have diabetes. Carb counting helps you keep tight control of your blood sugar (glucose) level. It also gives you the flexibility to eat what you want. This can help you feel more in control and confident when managing your diabetes.
- Carb counting helps you keep your blood sugar at your target level.
- It allows you to adjust the amount of insulin you take. This amount is based on how many grams of carbs you eat at a meal or snack. The formula used to find how much insulin you need is called the insulin-to-carbohydrate ratio.
- The insulin-to-carbohydrate ratio is not the same for each person. You and your doctor will find your ratio by keeping track of the food you eat and testing your blood sugar level after meals.
How do you count carbohydrate grams in your diet?
To count carb grams at a meal, you need to know how many carbs are in each type of food you eat. This includes all food, whether it is a slice of bread, a bowl of lettuce, or a spoonful of salad dressing. Most packaged foods have labels that tell you how many total carbs are in one serving. Carbohydrate guides can help too. You can get these from diabetes educators and the American Diabetes Association.
To find out how many carbs are in food that is not packaged, you will need to know standard portions of carbohydrate foods. Each serving size or standard portion has about 15 grams of carbs.
By using the number of grams of carbs in a meal, you can figure out how much insulin to take. This is based on your personal insulin-to-carbohydrate ratio.
For example: Your doctor may advise you to take 1 unit of rapid-acting insulin for every 10 to 15 grams of carbs you eat. So if your meal has 50 grams of carbs and your doctor says you need 1 unit of insulin for every 10 grams of carbs, you would need 5 units of insulin to keep your post-meal blood sugar from rising above your target level.
Your insulin-to-carbohydrate ratio may change over time. In some people it will change from one meal to the next. You might take 1 unit of insulin for every 10 grams of carbs for lunch but take 1 unit for every 15 grams at dinner.
Keep these tips in mind when counting carbs:
- Portion control is important. If a package says it contains two servings and you eat the whole package, you need to double the number of grams of carbs listed for one serving.
- Protein, fat, and fiber do not raise blood sugar very much. If you eat a lot of these nutrients in a meal, carbs will change to glucose more slowly than it would with a meal that has a small amount of protein, fat, and fiber.
- Advanced carb counting takes into account the amount of fiber or sugar alcohols in a food. For example, if a food has 5 or more grams of fiber per serving, you can subtract half the amount of fiber from the total number of carb grams. A food that has 30 grams of carbs and 8 grams of fiber would be counted as 26 grams of carbs. If you use a rapid-acting insulin, you may want to consider sugar alcohols if there are more than 5 grams of them in the food. Divide the number of sugar alcohols in half. Then subtract that number from the total carb count.
- Exercise affects blood sugar. It allows you to use less insulin than you would if you did not exercise. Keep in mind that timing makes a difference. If you exercise within 1 hour of a meal, your body may need less insulin for that meal than it would if you exercised 3 hours after the meal.
When you keep track of what you eat and you test your blood sugar after meals and exercise, you can figure out what effect protein, fat, fiber, and exercise have on the amount of insulin you need.
To count carbs and eat a balanced diet:
- Talk with a registered dietitian. He or she can help you plan how many carbs to include in each meal and snack. This includes sweets.
- Measure your food portions. You won’t always have to measure your food. But it may help when you are first learning what makes up a standard portion.
- Count either grams or servings of carbs.
- Eat standard portions of foods that have protein. Foods that have protein (such as beans, eggs, meat, and cheese) are a key part of a balanced diet.
- Limit saturated fats. A balanced diet includes a limited amount of healthy fat. Talk with a registered dietitian about how much fat you need in your diet.
Know your daily amount
Your daily amount depends on several things—your weight, how active you are, what diabetes medicines you take, and what your goals are for your blood sugar levels. A registered dietitian or certified diabetes educator will help you plan how much carbohydrate to include in each meal and snack.
For most adults, a guideline for the daily amount of carbohydrate is:
- 45 to 60 grams at each meal. That’s about the same as 3 to 4 carbohydrate servings.
- 15 to 20 grams at each snack. That’s about the same as 1 carbohydrate serving.
Other helpful ideas
- Read food labels for carb amounts. Be aware of the serving size on the package.
- Check your blood sugar level. If you do this before and 1 hour after a meal, you will be able to see how the food you eat affects your blood sugar.
- Record what you eat and your blood sugar results in a food record. You can review your food record each time you visit your registered dietitian or certified diabetes educator. And you can review it anytime you think your meal plan needs adjusting.
- Get more help. The American Diabetes Association offers booklets to help people learn how to count carbs in their diet. These booklets can also teach you how to measure and weigh food and to read food labels. But you will still need to talk with a registered dietitian to make a plan that fits your needs.
References
Other Works Consulted
- American Diabetes Association (2013). Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care, 36(11): 3821–3842. DOI: 10.2337/dc13-2042. Accessed December 5, 2013.
- Campbell AP, Beaser RS (2010). Medical nutrition therapy. In RS Beaser, ed., Joslin’s Diabetes Deskbook: A Guide for Primary Care Providers, 2nd ed., pp. 91–136. Boston: Joslin Diabetes Center.
- Franz MJ (2012). Medical nutrition therapy for diabetes mellitus and hypoglycemia of nondiabetic origin. In LK Mahan et al., eds., Krause’s Food and the Nutrition Care Process, 13th ed., pp. 675–710. St Louis: Saunders.
Credits
Current as of: April 16, 2019
Author: Healthwise Staff
Medical Review:E. Gregory Thompson MD – Internal Medicine & Kathleen Romito MD – Family Medicine & Adam Husney MD – Family Medicine & Rhonda O’Brien MS, RD, CDE – Certified Diabetes Educator & Colleen O’Connor PhD, RD – Registered Dietitian
Current as of: April 16, 2019
Author: Healthwise Staff
Medical Review:E. Gregory Thompson MD – Internal Medicine & Kathleen Romito MD – Family Medicine & Adam Husney MD – Family Medicine & Rhonda O’Brien MS, RD, CDE – Certified Diabetes Educator & Colleen O’Connor PhD, RD – Registered Dietitian
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.