Giant Cell Arteritis
Topic Overview
What is giant cell arteritis?
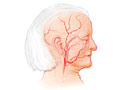
Giant cell arteritis (say “ar-tuh-RY-tus”), or GCA, is inflammation of the blood vessels. It mostly affects the arteries that carry blood to the head, especially those that supply the eyes, temple, and jaw. Because it often affects the artery in the temple, it is also called temporal arteritis.
People who have giant cell arteritis need to be treated right away. That’s because it can cause loss of vision and may lead to a stroke or mini-strokes.
Some people who have giant cell arteritis also have polymyalgia rheumatica. This is another inflammatory condition that affects the muscles. It causes pain and stiffness in the hip, neck, or shoulder area. The same medicines are used to treat both conditions.
What causes giant cell arteritis?
Experts don’t fully understand what causes it. It may be that the immune system is attacking the body’s own tissues. Your genes may play a role in this. For example, people whose ancestors are from Scandinavia or Northern Europe are more likely to have this problem.
Giant cell arteritis occurs in women more often than men. It is more common as people get older.
What are the symptoms?
Symptoms may start either suddenly or slowly. They may include:
- A new headache, often near the temple or around the eye. This is the most common symptom.
- Pain in the jaw, especially when you chew.
- Vision problems such as double vision or brief loss of vision.
- Tenderness on the side of the head or scalp. The blood vessel on the temple may look swollen. And it may hurt to wear glasses or comb your hair.
How is giant cell arteritis diagnosed?
Your doctor will do a physical exam and ask you about your symptoms and past health. For example, the doctor may look for arteries on the temple or forehead that are swollen, lumpy, or tender. This is a sign of giant cell arteritis.
The doctor will also consider your age in diagnosing this condition. People younger than 50 very rarely have giant cell arteritis.
The doctor may order tests too. These may include:
- Blood tests such as sedimentation rate and C-reactive protein. These tests can show if you have inflammation in your body.
- Complete blood count. This test can show if you have anemia, which is common in people who have giant cell arteritis.
- Temporal artery biopsy. For this test, a surgeon takes a small tissue sample from a blood vessel in your temple and checks it for inflammation.
Some other conditions can cause similar symptoms. Your doctor may also do tests to rule out those conditions, which include arthritis and hypothyroidism.
How is it treated?
Giant cell arteritis is treated with steroid medicines, which reduce inflammation. Giant cell arteritis is dangerous because it can cause serious problems, such as stroke or blindness. So your doctor may start you on the medicine right away, even before the diagnosis is confirmed.
You’ll probably feel better in a day or two after you start the medicine. Most of the time, symptoms improve quickly and go away 2 to 4 weeks after treatment starts. But you may need to keep taking steroid medicine for 1 to 2 years or even longer. This helps to keep your symptoms from coming back.
Long-term treatment with steroid medicine will put you at risk for bone thinning (osteoporosis). This is because steroid medicines reduce how well your body takes in calcium, which is important in building strong bones. Your doctor may recommend a bone density test to see if you need to take a medicine to prevent osteoporosis. These medicines are called bisphosphonates. Or your doctor may simply start you on the medicine without the test.
Your doctor may also suggest that you take:
- Medicine to help protect your digestive tract, such as a proton pump inhibitor or an H2 blocker. Taking medicines like steroids for a long time can irritate your esophagus and stomach and lead to ulcers. Proton pump inhibitors and H2 blockers help reduce this irritation.
- Aspirin. Some studies show that taking aspirin may reduce the risk of vision loss, stroke, and mini-strokes.
In some people, symptoms improve with treatment but then come back. This is called a relapse. It often occurs in the first 2 years of treatment or during the first year after steroid medicine is stopped. Your doctor will track your condition during this time. If you have a relapse, your doctor will increase the steroid dosage for a while. Then you can slowly lower it after your symptoms go away.
In rare cases, giant cell arteritis may affect the main part of the aorta, a large blood vessel in the chest. This can cause an aortic aneurysm, which can be life-threatening. Your doctor may want you to have chest X-ray each year to watch for this problem.
What can you do to stay healthy during treatment?
To protect your bones while you are being treated with steroid medicines:
- Be sure you get enough calcium and vitamin D. Calcium can help prevent bone thinning. Vitamin D helps your body absorb calcium.
- Ask your doctor if you need to take calcium and vitamin D supplements. Calcium supplements may interfere with your body’s ability to absorb bisphosphonates. So take your calcium and vitamin D supplement at least 30 minutes after you take your bisphosphonate.
- Get regular weight-bearing exercise, such as walking, dancing, or weight lifting. This will help keep your bones strong and may also help your mood.
- Don’t smoke, and avoid being around tobacco smoke.
- Limit alcohol. It’s a good idea to have no more than one beer or one glass of wine each day.
References
Other Works Consulted
- Both M, et al. (2006). Balloon angioplasty of arteries of the upper extremities in patients with extracranial giant-cell arteritis. Annals of the Rheumatic Diseases, 65(9): 1124–1130.
- Hellmann DB (2013). Giant cell arteritis, polymyalgia rheumatica, and Takayasu’s arteritis. In GS Firestein et al., eds., Kelley’s Textbook of Rheumatology, 9th ed., vol. 2, pp. 1461–1480. Philadelphia: Saunders.
- Hellmann DB, Imboden JB Jr (2012). Musculoskeletal and immunologic disorders. In SJ McPhee, MA Papadakis, eds., 2012 Current Medical Diagnosis and Treatment, 51st ed., pp. 787–846. New York: McGraw-Hill.
- Spiera RF (2016). Polymyalgia rheumatica and temporal arteritis. In L Goldman, A Shafer, eds., Goldman-Cecil Medicine, 24th ed., vol. 2, pp. 1801–1805. Philadelphia: Saunders.
Current as of: April 1, 2019
Author: Healthwise Staff
Medical Review:Anne C. Poinier, MD – Internal Medicine & Martin J. Gabica, MD – Family Medicine & E. Gregory Thompson, MD – Internal Medicine & Kathleen Romito, MD – Family Medicine
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.