Heart Failure
Topic Overview

What is heart failure?
Heart failure means that your heart muscle doesn’t pump as much blood as your body needs. Failure doesn’t mean that your heart has stopped. It means that your heart is not pumping as well as it should.
Because your heart cannot pump well, your body tries to make up for it. To do this:
- Your body holds on to salt and water. This increases the amount of blood in your bloodstream.
- Your heart beats faster.
- Your heart may get bigger.
Your body has an amazing ability to make up for heart failure. It may do such a good job that you don’t know you have a disease. But at some point, your heart and body will no longer be able to keep up. Then fluid starts to build up in your body, and you have symptoms like feeling weak and out of breath.
This fluid buildup is called congestion. It’s why some doctors call the disease congestive heart failure.
Heart failure usually gets worse over time. But treatment can slow the disease and help you feel better and live longer.
What causes heart failure?
Anything that damages your heart or affects how well it pumps can lead to heart failure. Common causes of heart failure are:
- High blood pressure.
- Heart attack.
- Coronary artery disease.
Other conditions that can lead to heart failure include:
- Diabetes.
- Diseases of the heart muscle (cardiomyopathies).
- Heart valve disease.
- Disease of the sac around the heart (pericardial disease), such as pericarditis.
- A slow, fast, or uneven heart rhythm (arrhythmia).
- A heart problem that you were born with (congenital heart defect).
- Long-term heavy alcohol use, which can damage your heart.
What are the symptoms?
Symptoms of heart failure start to happen when your heart cannot pump enough blood to the rest of your body. In the early stages, you may:
- Feel tired easily.
- Be short of breath when you exert yourself.
- Feel like your heart is pounding or racing (palpitations).
- Feel weak or dizzy.
As heart failure gets worse, fluid starts to build up in your lungs and other parts of your body. This may cause you to:
- Feel short of breath even at rest.
- Have swelling (edema), especially in your legs, ankles, and feet.
- Gain weight. This may happen over just a day or two, or more slowly.
- Cough or wheeze, especially when you lie down.
- Feel bloated or sick to your stomach.
If your symptoms suddenly get worse, you will need emergency care.
How is heart failure diagnosed?
Your doctor may diagnose heart failure based on your symptoms and a physical exam. But you will need tests to find the cause and type of heart failure so that you can get the right treatment. These tests may include:
- Blood tests.
- A chest X-ray.
- An electrocardiogram (EKG or ECG) to check your heart’s electrical system.
- An echocardiogram to see the size and shape of your heart and how well it is pumping.
- Magnetic resonance imaging (MRI) to see the structure of your heart and check how well it is pumping.
Echocardiogram
An echocardiogram can help show if you have heart failure, what type it is, and what is causing it. Your doctor can also use it to see if your heart failure is getting worse.
This test can measure how much blood your heart pumps to your body. This measurement is called the ejection fraction. If your ejection fraction gets lower and you are having more symptoms, it means that your heart failure is getting worse.
How is it treated?
Most people with heart failure need to take several medicines. Your doctor may prescribe medicines to:
- Help keep heart failure from getting worse. These drugs include ACE inhibitors, angiotensin II receptor blockers (ARBs), beta-blockers, and vasodilators like hydralazine and a nitrate.
- Reduce symptoms so you feel better. These drugs include diuretics (water pills) and digoxin.
- Treat the cause of your heart failure.
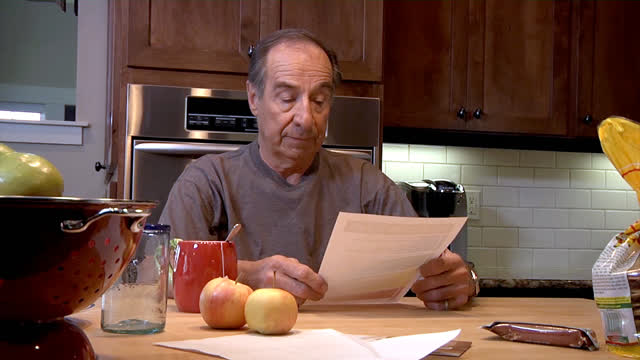
It is very important to take your medicines exactly as your doctor tells you to. If you don’t, your heart failure could get worse.
Pacemaker or defibrillator
A pacemaker or a defibrillator (such as an ICD) may be an option for you if you have a problem with your heart rhythm. A pacemaker can help your heart pump blood better. A defibrillator can prevent a dangerous heart-rhythm problem.
Care at home
Lifestyle changes are an important part of treatment. They can help slow down heart failure. They may also help control other diseases that make heart failure worse, such as high blood pressure, diabetes, and coronary artery disease.
The best steps you can take are to:
- Eat less sodium. Sodium causes your body to hold on to water and may make symptoms worse. Your doctor may also ask you to limit how much fluid you drink.
- Get regular exercise. Your doctor can tell you what level of exercise is safe for you, how to check your pulse, and how to know if you are doing too much.
- Take rest breaks during the day.
- Lose weight if you are overweight. Even a few pounds can make a difference.
- Stop smoking. Smoking damages your heart and makes exercise harder to do.
- Limit alcohol. Ask your doctor how much, if any, is safe.
Ask your doctor if cardiac rehab is right for you. Rehab can give you education and support that help you learn self-care and build new healthy habits, such as exercise and healthy eating.
To stay as healthy as possible, work closely with your doctor. Have all your tests, and go to all your appointments. It is also important to:
- Talk to your doctor before you take any new medicine, including nonprescription and prescription drugs, vitamins, and herbs. Some of them may make your heart failure worse.
- Keep track of your symptoms. Weigh yourself at the same time every day, and write down your weight. Call your doctor if you have a sudden weight gain, a change in your ability to exercise, or any sudden change in your symptoms.
What can you expect if you have heart failure?
Medicines and lifestyle changes can slow or even reverse heart failure for some people. But heart failure often gets worse over time.
Early on, your symptoms may not be too bad. As heart failure gets worse, you may need to limit your activities. Treatment can often help reduce symptoms, but it usually doesn’t get rid of them.
Heart failure can also lead to other health problems. These may include:
- Trouble with your heart rhythm (arrhythmia).
- Stroke.
- Heart attack.
- Mitral valve regurgitation.
- Blood clots in your legs (deep vein thrombosis) or lungs (pulmonary embolism).
Your doctor may be able to give you medicine or other treatment to prevent or treat these problems.
Heart failure can get worse suddenly. If this happens, you will need emergency care. To prevent sudden heart failure, you need to avoid things that can trigger it. These include eating too much salt, missing a dose of your medicine, and exercising too hard.
Knowing that your health may get worse can be hard. It is normal to sometimes feel sad or hopeless. But if these feelings last, talk to your doctor. Antidepressant medicines, counseling, or both may help you cope.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
- Anxiety: Stop Negative Thoughts
- Blood Thinners Other Than Warfarin: Taking Them Safely
- Depression: Stop Negative Thoughts
- Healthy Eating: Eating Less Sodium
- Heart Failure: Activity and Exercise
- Heart Failure: Avoiding Medicines That Make Symptoms Worse
- Heart Failure: Avoiding Triggers for Sudden Heart Failure
- Heart Failure: Checking Your Weight
- Heart Failure: Taking Medicines Properly
- Heart Failure: Watching Your Fluids
- Insomnia: Improving Your Sleep
- Low-Salt Diets: Eating Out
- Stop Negative Thoughts: Getting Started
- Stress Management: Breathing Exercises for Relaxation
- Stress Management: Doing Guided Imagery to Relax
- Stress Management: Doing Meditation
- Stress Management: Doing Progressive Muscle Relaxation
- Stress Management: Managing Your Time
- Stress Management: Practicing Yoga to Relax
- Warfarin: Taking Your Medicine Safely
Cause
Heart failure can be caused by any problem that damages your heart or affects how well it works.
Problems that damage the heart muscle
- High blood pressure
- Heart attack
- Coronary artery disease
- Diabetes that isn’t controlled
- Alcohol, illegal drugs (such as cocaine), and some prescription medicines (such as those for chemotherapy)
- Heart problems you’ve had from birth (congenital heart disease)
- Infection or inflammation of the heart muscle (such as myocarditis)
Things that damage the heart’s valves
- Valve problems you’ve had since birth
- Infection of a heart valve (endocarditis)
- Aging
- Rheumatic fever
Problems with the heart’s electrical system
- Fast, slow, or irregular heart rhythms, including atrial fibrillation
- Electrical signals that don’t flow as they should from the upper to the lower part of the heart (heart block)
Other problems
- Disease of the sac around the heart (pericarditis)
- Postpartum cardiomyopathy. This rare problem can happen late in a woman’s pregnancy or within the first 5 months after delivery.
- Severe anemia
- Hyperthyroidism
Certain triggers, such as too much sodium or not taking medicines the right way, may suddenly make heart failure worse. This can sometimes cause deadly problems such as pulmonary edema or cardiogenic shock.
Symptoms
At first you may not have any symptoms from heart failure. For a while, your heart and body can make up for heart failure. For example, your heart can pump faster and pump more blood with each beat. This is called compensation.
But as your heart has more trouble pumping enough blood to your body, you will likely have symptoms. These symptoms may get worse or change if your heart failure gets worse.
Symptoms of heart failure start to happen when your heart can’t pump enough blood to the rest of your body. In the early stages, you may:
- Feel tired easily.
- Be short of breath when you exert yourself.
- Feel like your heart is pounding or racing (palpitations).
- Feel weak or dizzy.
As heart failure gets worse, fluid starts to build up in your lungs and other parts of your body. This may cause you to:
- Feel short of breath even at rest.
- Have swelling (edema), especially in your legs, ankles, and feet.
- Gain weight. This may happen over just a day or two, or more slowly.
- Cough or wheeze, especially when you lie down.
- Feel bloated or sick to your stomach.
How doctors talk about heart failure
There is more than one type of heart failure. Each type is based on what problem in the heart is causing it to not pump as much blood as normal.
Heart failure is grouped—or classified—according to symptoms. Your treatment is based partly on what class of symptoms you have.
There’s also another way to define heart failure. It’s based on the stages you might go through as your heart failure gets worse. Your doctor also may make treatment choices based on your stage of heart failure.
Symptoms of sudden heart failure
Sometimes your symptoms may get worse very quickly. This is called sudden heart failure. It causes fluid to build up in your lungs, causing congestion. (This is why the problem is often called congestive heart failure.) Symptoms may include:
- Severe shortness of breath.
- An irregular or fast heartbeat.
- Coughing up foamy, pink mucus.
Sudden heart failure is an emergency. You need care right away.
More information
What Increases Your Risk
Your risk for having heart failure is higher if you have certain risk factors. A risk factor is anything that increases your chance of having a particular problem.
Heart failure is usually caused by another health problem, often coronary artery disease or high blood pressure. So anything that increases your risk for one of those problems also increases your risk for heart failure.
- Risk factors for coronary artery disease and heart attack include smoking, having high cholesterol or diabetes, and having a family history of heart disease.
- Risk factors for high blood pressure include being overweight, being inactive, and having a family history of high blood pressure.
- Risk factors for heart valve disease include older age and an infection of the valves.
The risk of heart failure rises as a person gets older.
When to Call a Doctor
Call 911 or other emergency services right away if you have:
- Symptoms of sudden heart failure, such as:
- Severe shortness of breath (trouble getting a breath even when resting).
- Suddenly getting an irregular heartbeat that lasts for a while, or getting a very fast heartbeat along with dizziness, nausea, or fainting.
- Foamy, pink mucus with a cough and shortness of breath.
- Symptoms of a heart attack, such as:
- Chest pain or pressure, or a strange feeling in the chest.
- Sweating.
- Shortness of breath.
- Nausea or vomiting.
- Pain, pressure, or a strange feeling in the back, neck, jaw, or upper belly, or in one or both shoulders or arms.
- Lightheadedness or sudden weakness.
- A fast or irregular heartbeat.
- Symptoms of a stroke. These include:
- Sudden numbness, tingling, weakness, or paralysis in your face, arm, or leg, especially on only one side of your body.
- Sudden vision changes.
- Sudden trouble speaking.
- Sudden confusion or trouble understanding simple statements.
- Sudden problems with walking or balance.
- A sudden, severe headache that is different from past headaches.
Call your doctor right away if you have a pacemaker or ICD and think you have an infection near the device. Signs of an infection include:
- Changes in the skin around your pacemaker or ICD, such as:
- Swelling.
- Warmth.
- Redness.
- Pain.
- Fever not caused by the flu or another illness.
Call your doctor soon if you have symptoms of heart failure, which include:
- Being very tired or having weakness that prevents you from doing your usual activities.
- Having breathing problems such as:
- Trouble breathing during routine activities or exercise that did not cause problems before.
- Sudden shortness of breath, even if it is mild.
- Shortness of breath when you lie down.
- Waking up at night with shortness of breath or feeling as though you are suffocating.
- A dry, hacking cough, especially when you lie down.
- Sudden weight gain, such as more than 2 lb (0.9 kg) to 3 lb (1.4 kg) in a day or 5 lb (2.3 kg) in a week. (Your doctor may suggest a different range of weight gain.)
- Increased fluid buildup in your body (most often in the legs).
Call your doctor soon if:
- Your heart failure symptoms get worse.
- You have a sudden change in symptoms.
- You’re having trouble keeping even minor symptoms under control.
Who to see
Many different types of doctors and nurses can treat you for heart failure, including your family doctor.
Exams and Tests
Heart failure is a complex problem. So you will likely have several different tests over time. These tests can:
- Find out if you have heart failure.
- Find the cause of your heart failure.
- Find the type of heart failure you have.
- Show how bad your heart failure is (class and stage).
- See how well your treatment is working.
If you have symptoms that suggest heart failure, you may have:
- A review of your medical history and a physical exam.
- Blood tests.
- Electrocardiogram (EKG, ECG).
- Chest X-ray.
- Echocardiogram (echo).
- Brain natriuretic peptide (BNP).
- Magnetic resonance imaging (MRI).
- Cardiac blood pool scan.
An echocardiogram may be used to diagnose heart failure. It also can help guide treatment.
Tests also may be done to find areas of the heart that are not getting enough blood. These tests include:
- Cardiac perfusion scan. This test can show poor blood flow to the heart.
- Cardiac catheterization. This test can be used to check for blocked or narrowed heart arteries and to measure pressures inside the heart.
When you’re taking medicine for heart failure, you may have regular blood tests to check how the medicine is working. Or you may have a blood test to check the level of medicine in your body.
More information
- How Often You’ll See Your Doctor for Heart Failure
- Heart Failure With Reduced Ejection Fraction (Systolic Heart Failure)
- Heart Failure With Preserved Ejection Fraction (Diastolic Heart Failure)
- Right-Sided Heart Failure
- High-Output Heart Failure
Treatment Overview
Your treatment for heart failure depends on:
- The cause of your heart failure.
- Which type of heart failure you have.
- How bad your symptoms are (classification).
- How well your body is able to make up (compensate) for your heart failure.
- Your goals, wishes, and preferences about your treatment.
In the early stages of heart failure, treatment can help your symptoms. It may also prevent more damage to your heart. Treatment may include:
- Taking medicines, such as a diuretic and an ACE inhibitor. To learn more, see Medications.
- Making lifestyle changes, such as eating less salt and being more active. To learn more, see Living With Heart Failure.
As part of your ongoing treatment, your doctor will also try to prevent or treat problems—such as fever, arrhythmia, and anemia—that can lead to sudden heart failure. Treatment may include:
- Getting vaccines. Your doctor may want you to get vaccines against pneumonia and flu. These vaccines can keep you from getting infections that could put you in the hospital.
- Checking your weight. Your doctor will probably give you guidelines for watching fluid buildup and tell you how much weight gain is too much.
- Getting devices to fix heart rhythm problems. In some cases, your doctor may recommend a biventricular pacemaker that can help your heart pump blood better. This is also called cardiac resynchronization therapy (CRT). Or you may have an implantable cardioverter-defibrillator (ICD) to stop a deadly rhythm. Some people get a pacemaker that is combined with an ICD.
- Oxygen treatment. Your doctor may recommend oxygen therapy to reduce your shortness of breath and increase your ability to exercise.
You might take part in a disease management program. These programs include a broad range of services, such as education, home health care, visiting nurses, and rehabilitation.
A very small number of people may have other treatments, including:
- Ventricular assist devices (VADs), which help the heart pump blood.
- Heart transplant, which replaces your heart with a donor heart.
Treatment for causes of heart failure
If you have other heart problems that may have led to heart failure, you might have treatment for those problems:
- Coronary artery bypass surgery or angioplasty.
- Surgery to replace or repair a valve in your heart.
- Cardiac rehabilitation, a supervised program that uses exercise, education, and support to help people live well with heart failure. For more information, see the topic Cardiac Rehabilitation.
Sometimes heart failure can be fixed if another problem can be corrected, such as by treating hyperthyroidism.
Palliative care
Palliative care is a kind of care for people who have a serious illness. It’s different from care to cure your illness. Its goal is to improve your quality of life—not just in your body but also in your mind and spirit.
You can have this care along with treatment to cure your illness. You can also have it if treatment to cure your illness no longer seems like a good choice.
Palliative care providers will work to help control pain or side effects. They may help you decide what treatment you want or don’t want. And they can help your loved ones understand how to support you.
If you’re interested in palliative care, talk to your doctor.
For more information, see the topic Palliative Care.
End-of-life care
Heart failure tends to get worse over time. So you need to decide what kind of care you want at the end of your life.
It can be hard to have talks with your doctor and family about the end of your life. But making these decisions now may bring you and your family peace of mind. Your family won’t have to wonder what you want. And you can spend your time focusing on your relationships.
You will need to decide if you want life-support measures if your health gets very bad. An advance directive is a legal document that tells doctors how to care for you at the end of your life. This care includes electronic devices that are used for heart failure, such as pacemakers. You also can say where you want to have care. And you can name someone who can make sure your wishes are followed.
For more information, see the topic Care at the End of Life.
Prevention
The best way to prevent heart failure is to have a heart-healthy lifestyle and control existing health problems like high blood pressure and diabetes.
To reduce your risk:
- Don’t smoke. If you smoke, quit. Avoid secondhand smoke too.
- Eat heart-healthy foods. Eat fruits, vegetables, fish, lean meats, and whole grains. Choose foods that are low in saturated fat and avoid trans fat. Limit sodium, alcohol, and sugar.
- Get regular exercise. Try to do activities that raise your heart rate. Aim for at least 2½ hours of moderate exercise a week.footnote 1
- Stay at a healthy weight. Lose weight if you need to.
- Manage other health problems that can raise your risk of heart disease and heart failure. These include high blood pressure, high cholesterol, and diabetes. You can use heart-healthy lifestyle changes along with medicines to manage these conditions.
Living With Heart Failure
You can feel better when you have heart failure by taking your medicines as directed, having a healthy lifestyle, and avoiding things that make heart failure worse. Know what things you can do every day to stay healthy, what symptoms to watch for, and when to call a doctor.
Ask your doctor if cardiac rehab is right for you. Rehab can give you education and support that help you learn self-care and build new healthy habits, such as exercise and healthy eating.
Taking medicines
- Take your medicines as directed. If you don’t, your heart failure may get worse, or you may get sudden heart failure.
- Try to avoid medicines that can make your heart failure worse. Before taking any new medicine, ask your doctor or a pharmacist if it’s safe to take it with your heart failure medicines.
Having a healthy lifestyle
- Eat healthy foods.
- Limit sodium. Your doctor might recommend that you limit sodium to less than 2,000 mg a day. Limiting sodium can help you feel better and prevent sudden heart failure. Fluid may build up in your lungs—making it harder for you to breathe—and in your feet, ankles, legs, and belly.
- Exercise regularly. If you aren’t already active, your doctor may want you to start exercising. Do not start exercising until you have talked with your doctor to make an exercise program that is safe for you. You could do it in a cardiac rehabilitation program or on your own.
- Check your weight at the same time every day. Checking your weight helps you keep track of your symptoms. Sudden weight gain may mean that fluid is building up in your body because your heart failure is getting worse.
- Try to lose weight if you are overweight. Eating a heart-healthy diet and exercising regularly will help you lose weight. Even a few pounds can make a difference.
- Don’t smoke. If you smoke, try to quit. Smoking increases your risk for heart disease and makes it harder to exercise. Avoid secondhand smoke too.
- Limit alcohol. Moderate drinking is no more than 2 drinks a day for men and 1 drink a day for women.
- Limit your fluids if your doctor tells you to. Limiting fluid can help relieve swelling. Limiting fluid helps your body get rid of extra water and sodium.
- Oxygen treatment. Your doctor may recommend oxygen therapy to reduce your shortness of breath and increase your ability to exercise.
Avoiding things that make heart failure worse
Avoid triggers, such as too much salt (sodium) and certain medicines, that can cause sudden heart failure.
Treating your sleep problems
 One Man’s Story: Pete, 70 “I was having a lot of trouble getting enough sleep. I was snoring so bad that my wife was sleeping in another room. I’d wake up 7 times a night. Sometimes I’d wake up gasping for breath. The next day I’d be so tired that I’d fall asleep while doing my woodworking in the garage. And I was really fuzzy-headed. I couldn’t remember anything. “I thought it might be my heart failure. So I decided to talk to my doctor about it, and he suggested a sleep study. I found out that I have sleep apnea. I haven’t been getting enough oxygen because of it. He put me on a CPAP machine at night. I’ve used it for the past 4 months. “It took a little time to get used to sleeping with a mask. But I’m sleeping much better. Now if I wake up, it’s only once, and I go right back to sleep. I feel so much better during the day.”— Pete This story is based on information gathered from many people living with heart failure. |
Many people with heart failure have trouble sleeping. Your doctor may be able to find out what is causing your sleep problems and help you get a good night’s sleep.
Having a healthy sex life
Most people with heart failure can still have an active and safe sex life. Talk with your doctor if you have concerns about having sex.
Unfortunately, sexual problems are common. Your interest may drop, or you may have shortness of breath or other symptoms that limit your ability to have sex. Men may have erection problems.
Talk to your doctor. You can get help for erection problems or other sexual troubles.
Other things you can do to take care of yourself
- Get help for depression and anxiety if you have them. Heart failure can be hard on your emotions. Many people with heart failure feel depressed or anxious. For more information on how to feel better, see Coping With Your Feelings.
- Try sometips for easier breathing, such as propping yourself up with pillows at night.
- Avoid colds and the flu.Stay up to date on vaccines for flu and pneumonia.
- Learn to save your energy to make activities like work, exercise, and travel easier. Talk to your doctor.
- Work with yourteam of health professionals.
Help for caregivers
It can be rewarding to help a loved one with heart failure. But it’s also a lot of work. And it can be hard emotionally.
If you are taking care of a loved one, make sure that you also take care of yourself. This can mean taking breaks by getting help from family or friends. You also may be able to use respite care. These services provide someone who will stay with your loved one while you get out of the house for a few hours.
More information
Coping With Your Feelings
Heart failure brings big changes to your life. You may struggle with sadness and worry. You may wonder if you’ll still be able to enjoy your life. Coping with your feelings and seeking help when you need it can help you live better with heart failure.
Depression and anxiety
Heart failure can be hard on your emotions. You may feel depressed that you can’t do some of the things you used to do. You may worry about your future. And symptoms of heart failure, such as shortness of breath, can make this anxiety worse.
These feelings are common. Talk to your doctor if you have symptoms of depression or are worried a lot. Depression and anxiety can be treated with counseling and medicine.
You also can help yourself feel better by changing your “self-talk.” Those are the things you tell yourself about how you’re coping. Negative thoughts can make you feel bad. Changing the way you think can change the way you feel.
 One Woman’s Story: Joan, 54 “I would sit at my kitchen table and feel I was in this cloud of dread. I didn’t feel like me. I felt like, ‘I’m never going to be me again.’ “— Joan Read about how Joan got help for depression and anxiety. |
For more information, see:
Stress
The challenges of living with heart failure can increase your stress. And stress can make living with heart failure even harder. Stress also can disturb your sleep and make depression and anxiety worse. Explore ways to relax and manage stress to help your body, mind, and spirit.
- Stress Management: Doing Progressive Muscle Relaxation
- Stress Management: Managing Your Time
- Stress Management: Reducing Stress by Being Assertive
- Stress Management: Breathing Exercises for Relaxation
- Stress Management: Doing Guided Imagery to Relax
- Stress Management: Doing Meditation
- Stress Management: Practicing Yoga to Relax
Getting support
Emotional support from friends and family can help you cope with the struggles of heart failure. You might want to think about joining a heart failure support group. Ask your doctor about the types of support that are available where you live.
Cardiac rehab programs can offer support for you and your family. Ask your doctor if rehab is right for you.
Meeting other people with the same problems can help you know you’re not alone. If you’re shy or aren’t a joiner, you can look at an online support group. Even though people online aren’t talking face-to-face, they’re sharing their feelings and creating a community.
Medications
You probably will need to take several medicines to treat heart failure, even if you don’t have symptoms yet.
Medicines don’t cure heart failure. But they can help your heart work better and improve symptoms.
Medicines can:
- Relieve or control symptoms.
- Treat other health problems you have, such as coronary artery disease.
- Improve your daily quality of life.
- Slow the rate at which your heart failure gets worse.
- Reduce the chance of other problems from heart failure, such as stroke.
- Reduce hospital stays.
- Help you live as long as possible.
It’s very important to take your medicines exactly as your doctor says. If you don’t, your heart failure may get worse or you may get sudden heart failure.
The medicines you take will depend on the type of heart failure you have. The most commonly used medicines are listed below.
Medicines for pumping problems (heart failure with reduced ejection fraction, or systolic heart failure)
- ACE inhibitors (angiotensin-converting enzyme inhibitors) relax and widen blood vessels. This makes it easier for blood to flow.
- Aldosterone receptor antagonists, a type of diuretic, make the kidneys get rid of extra fluid.
- ARBs (angiotensin II receptor blockers) make it easier for blood to flow through the vessels.
- ARNI (angiotensin receptor neprilysin inhibitor) medicine makes it easier for blood to flow through the vessels. ARNI medicine may be used instead of an ACE inhibitor or an ARB.
- Beta-blockers slow the heart rate. They also may help the heart fill with blood more completely.
- Digoxin helps the heart pump more blood with each beat.
- Diuretics help relieve symptoms like swelling in the legs.
- Hydralazine taken with a nitrate widens blood vessels. This medicine can lower blood pressure and reduce the workload on the heart.
- Ivabradine slows the heart rate. This medicine may help prevent some people from being hospitalized for heart failure.
Medicines for filling problems (heart failure with preserved ejection fraction, or diastolic heart failure)
Other medicines
You also may take other medicines for health problems that can cause heart failure or for problems caused by heart failure.
- Antiarrhythmics prevent very fast and sometimes irregular heart rhythms.
- Blood thinners, also known as anticoagulants, prevent dangerous blood clots.
Talk to your doctor before you take any over-the-counter medicines. Some of them might make your symptoms worse.
More information
Surgery
Surgeries for heart failure include:
- Surgery to get a pacemaker, implantable cardioverter-defibrillator (ICD), or ventricular assist device (VAD). For more information, see Other Treatment.
- Heart transplant to replace a failing heart. This is not common.
Other Treatment
Pacemakers
Cardiac resynchronization therapy (CRT) uses a biventricular pacemaker, which makes the heart’s lower chambers (ventricles) pump together. This can help your heart pump blood better. This type of pacemaker can help you feel better so you can be more active. It also can help keep you out of the hospital and help you live longer.
A pacemaker may be used alone or along with an implantable cardioverter-defibrillator (ICD) for heart failure.
Implantable defibrillators (ICDs)
Implantable cardioverter-defibrillators (ICDs) can prevent sudden death from an abnormal heart rhythm and may help you live longer. An ICD checks the heart for very fast and deadly heart rhythms. If the heart goes into one of these rhythms, the ICD shocks it to stop the deadly rhythm and returns the heart to a normal rhythm.
An ICD may be used alone or along with a pacemaker for heart failure.
Ventricular assist devices (VADs)
Ventricular assist devices (VADs), also known as heart pumps, may be placed into the chest to help the heart pump more blood. VADs can keep people alive until a donor heart is available for transplant. In some cases, VADs may also be used as an alternative to heart transplant for long-term treatment. VADs are used in people who have severe heart failure.
Intra-aortic balloon pump
An intra-aortic balloon pump is sometimes used to help the heart pump more blood during sudden heart failure.
Supplements
Talk to your doctor before you take any over-the-counter medicine or supplement. They are used along with medical treatments for heart failure, not instead of treatment.
You may hear about supplements, vitamins, or hormones that might improve heart failure symptoms.
Fish oil (omega-3 fatty acid) supplements have been shown to help some heart failure patients. In some studies, fish oil supplements, taken along with other heart failure medicines, helped people stay out of the hospital and live longer.footnote 2
No other supplement, vitamin, or hormone has been shown definitely to relieve heart failure or help you live longer.
Examples include coenzyme Q10 and hawthorn.
- Only some of the studies of coenzyme Q10 showed that it helps heart failure symptoms.footnote 3
- Hawthorn is an herb that is sometimes used in Europe and Asia to try to increase blood flow to the heart.
Related Information
- Heart Attack and Unstable Angina
- High Blood Pressure
- Care at the End of Life
- Reducing Medication Costs
- Quitting Smoking
- Cardiac Rehabilitation
- Coronary Artery Disease
- Questions to Ask About Your Medicines
- Dealing With Medicine Side Effects and Interactions
- Navigating Your Hospital Stay
- Atrial Fibrillation
References
Citations
- U.S. Department of Health and Human Services (2008). 2008 Physical Activity Guidelines for Americans (ODPHP Publication No. U0036). Washington, DC: U.S. Government Printing Office. Available online: http://www.health.gov/paguidelines/guidelines/default.aspx.
- Siscovick DS, et al. (2017). Omega-3 polyunsaturated fatty acid (fish oil) supplementation and the prevention of clinical cardiovascular disease: A science advisory from the American Heart Association. Circulation, 135(15): e867-e884. DOI: 10.1161/CIR.0000000000000482. Accessed April 10, 2017.
- Coenzyme Q10 (2006). Medical Letter on Drugs and Therapeutics, 48(1229): 19–20.
Other Works Consulted
- Allen LA, et al. (2012). Decision making in advanced heart failure: A scientific statement from the American Heart Association. Circulation, 125(15): 1928–1952.
- Drugs for treatment of chronic heart failure (2009). Treatment Guidelines From The Medical Letter, 7(83): 53–56.
- Levine GN, et al. (2012). Sexual activity and cardiovascular disease: A scientific statement from the American Heart Association. Circulation, 125(8): 1058–1072.
- McKelvie R (2011). Heart failure, search date August 2010. BMJ Clinical Evidence. Available online: http://www.clinicalevidence.com.
- Riegel B, et al. (2009). State of the science. Promoting self-care in patients with heart failure. A scientific statement from the American Heart Association. Circulation, 120(12): 1141–1163.
- Rosendorff C, et al. (2015). Treatment of hypertension in patients with coronary artery disease: A scientific statement from the American Heart Association, American College of Cardiology, and American Society of Hypertension. Circulation, 131(19): e435–e470. DOI: 10.1161/CIR.0000000000000207. Accessed March 31, 2015.
- Smith SC, et al. (2011). AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: A guideline from the American Heart Association and American College of Cardiology Foundation. Circulation, 124(22): 2458–2473. Also available online: http://circ.ahajournals.org/content/124/22/2458.full.
- Somers VK, et al. (2008). Sleep apnea and cardiovascular disease: An American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing in collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Circulation, 118(10): 1080–1111.
- Yancy CW, et al. (2013). 2013 ACCF/AHA Guideline for the management of heart failure: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology, 62(16): e147–e239.
- Yancy CW, et al. (2016). 2016 ACC/AHA/HFSA Focused update on new pharmacological therapy for heart failure: An update of the 2013 ACCF/AHA guideline for the management of heart failure. Circulation, published online May 20, 2016. DOI: 10.1161/CIR.0000000000000435. Accessed June 10, 2016.
Credits
Current as ofApril 9, 2019
Author: Healthwise Staff
Medical Review: Rakesh K. Pai MD, FACC – Cardiology, Electrophysiology
E. Gregory Thompson MD – Internal Medicine
Martin J. Gabica MD – Family Medicine
Elizabeth T. Russo MD – Internal Medicine
Adam Husney MD – Family Medicine
Kathleen Romito MD – Family Medicine
Stephen Fort MD, MRCP, FRCPC – Interventional Cardiology
Current as of: April 9, 2019
Author: Healthwise Staff
Medical Review:Rakesh K. Pai MD, FACC – Cardiology, Electrophysiology & E. Gregory Thompson MD – Internal Medicine & Martin J. Gabica MD – Family Medicine & Elizabeth T. Russo MD – Internal Medicine & Adam Husney MD – Family Medicine & Kathleen Romito MD – Family Medicine & Stephen Fort MD, MRCP, FRCPC – Interventional Cardiology
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.