Kidney Transplant
Surgery Overview
A kidney transplant is surgery to put a healthy (donor) kidney into your body. There are two types of donors:
- Living donors. A living donor may be a family member, a friend, a coworker, or any person who is willing to give a kidney to someone in need. A person only needs one healthy kidney to live.
- Deceased donors. A deceased donor is someone who has recently died.
You may need to have tests to see how well the donor kidney matches your tissue type and blood type. A close tissue match reduces the chances that your body will reject the new kidney. You will also be evaluated to make sure that you do not have significant heart or lung disease or other diseases, such as cancer, which might decrease your life span.
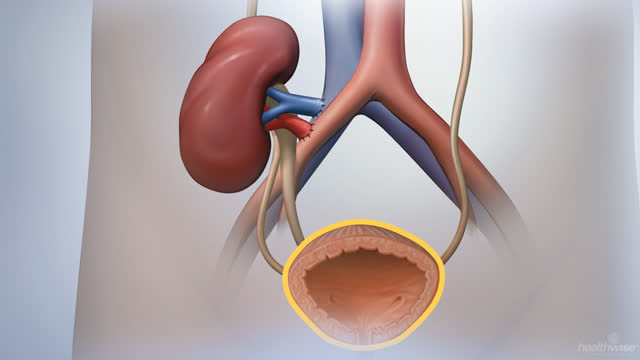
Kidney transplant surgery takes about 3 hours. During surgery, the donor kidney will be placed in your lower abdomen, blood vessels from the donor kidney will be connected to arteries and veins in your body, and the ureter from the donor kidney will be connected to your bladder. Blood is then able to flow through the new kidney, and the kidney will begin to filter and remove wastes and to produce urine.
The new kidney usually begins to function right away. In most cases, diseased or damaged kidneys are not removed unless you have a severe infection of the kidney (pyelonephritis), kidney cancer, nephrotic syndrome, or extremely large polycystic kidneys.
To learn more, see the topic Organ Transplant.
What To Expect
You will have to stay in the hospital for several days after you receive your new kidney. In some cases, it may take time for your new kidney to produce urine. So you may have to receive dialysis and take medicines, such as diuretics, that help your new kidney get rid of excess water and salt from your body.
After the surgery you will have to take medicines to suppress your immune system. These medicines are used to help keep your body from rejecting your new kidney. You will need to take these medicines for the rest of your life.
During the first weeks to months after your surgery, your body may try to reject your new kidney. This is called acute rejection and occurs in about 1 out of 10 people in the first year after transplant. Most of the time, acute rejection can be treated with antirejection (immunosuppressive) medicines.footnote 1
Chronic rejection (also called chronic allograft failure) is a process of gradual, progressive loss of kidney function and can occur many months to several years after your surgery. Experts don’t fully understand what causes chronic rejection. There is no treatment for chronic rejection. Most people go back on dialysis or have another transplant.
Why It Is Done
Kidney transplant surgery is done so that a healthy kidney (donor kidney) can do what your diseased kidney can no longer do. Kidney transplant is used when you have severe chronic kidney disease (renal failure) that cannot be reversed by another treatment method. You will not be able to have this surgery if you have an active infection, another life-threatening disease such as cancer, or severe heart or lung disease.
How Well It Works
If you have severe chronic kidney disease and choose to have a kidney transplant, you may live longer than if you choose only to treat your kidney disease with dialysis alone.
In the past, transplants using a kidney from a first-degree relative, such as your father, mother, brother, or sister, were the most successful. But with modern antirejection drugs, kidneys from people you are not related to work well, too. Transplants from living donors or from deceased donors can succeed.
Risks
The risks of having a kidney transplant include:
- Rejection of the new kidney.
- Severe infection.
- Bleeding.
- Reaction to the anesthesia used for surgery.
- Failure of the donor kidney.
What To Think About
Kidney transplant may be a better treatment for you than dialysis, because survival rates are better after transplant. You will also be able to live a more normal life, because you won’t have to have dialysis. Although a kidney transplant is an expensive procedure, it may actually be less costly than long-term dialysis treatments.
There is often a long wait before you receive a donor kidney. And there is no guarantee that the transplant will be successful. Fewer complications occur in people who are good candidates for surgery and who do not have other serious medical conditions, such as unstable coronary artery disease or cancer, that may limit their life expectancy.
Not everyone is able to have a kidney transplant. You will not usually have a kidney transplant if you have an active infection or another life-threatening disease, such as cancer or significant heart or lung disease.
After having a kidney transplant, you will have to take medicines that suppress your immune system (antirejection or immunosuppressive medicines) to help prevent your body from rejecting the new kidney. You will need to take these medicines for the rest of your life. Because these medicines weaken your immune system, you will have an increased risk for serious infections. There is also the chance that your body may still reject your new kidney even if you take these medicines. If this happens, you will have to start dialysis and possibly wait for another kidney transplant.
Immunosuppressive medicines also increase your risk of other diseases, such as skin cancer and lymphoma. You have a greater risk for diabetes, high blood pressure, heart disease, cataracts, and inflammation of the liver (cirrhosis) if you are taking these medicines.
References
Citations
- Hart A, et al. (2017). OPTN/SRTR 2015 annual data report: Kidney. American Journal of Transplantation, 17(Suppl 1): 21-116. DOI: 10.1111/ajt.14124. Accessed April 26, 2017.
Other Works Consulted
- Barry JM, Conlin MJ (2012). Renal transplantation. In AJ Wein et al., eds., Campbell-Walsh Urology, 10th ed., vol. 2, pp. 1226–1253. Philadelphia: Saunders.
- Flechner SM (2013). Renal transplantation. In JW McAninch, TF Lue, eds., Smith and Tanagho’s General Urology, 18th ed., pp. 550–569. New York: McGraw-Hill.
Credits
Current as of: December 12, 2018
Author: Healthwise Staff
Medical Review:Anne C. Poinier, MD – Internal Medicine & Adam Husney, MD – Family Medicine & Elizabeth T. Russo, MD – Internal Medicine
Current as of: December 12, 2018
Author: Healthwise Staff
Medical Review:Anne C. Poinier, MD – Internal Medicine & Adam Husney, MD – Family Medicine & Elizabeth T. Russo, MD – Internal Medicine
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.