Rheumatoid Arthritis
Topic Overview

Is this topic for you?
There are many types of arthritis (disease of the joints). This topic is about rheumatoid arthritis. If you are looking for information about how juvenile idiopathic (rheumatoid) arthritis affects young children, see the topic Juvenile Idiopathic Arthritis. If you are looking for information on the most common form of arthritis in older adults, see the topic Osteoarthritis.
What is rheumatoid arthritis?
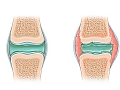
Rheumatoid arthritis (RA) causes the joints to become swollen, stiff, and painful (inflamed).
Over time, this inflammation may destroy the joint tissues. This can limit your daily activities and make it hard for you to walk and use your hands.
Rheumatoid arthritis is more common in women than in men. It often begins between the ages of 40 and 60.
What causes rheumatoid arthritis?
The exact cause is not known. But rheumatoid arthritis is an autoimmune disease. This means that the body’s natural defense system attacks the joints. The disease may run in some families.
What are the symptoms?
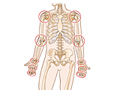
The main symptoms of rheumatoid arthritis are pain, stiffness, and swelling in the joints of the hands, wrists, elbows, feet, ankles, knees, or neck. The disease usually affects both sides of the body at the same time. In rare but severe cases, it may affect the eyes, lungs, heart, nerves, or blood vessels.
Sometimes the disease can cause bumps called nodules to form over the elbows, knuckles, spine, and lower leg bones.
How is rheumatoid arthritis diagnosed?
There is no single test for rheumatoid arthritis. Your doctor will do a physical exam and look at your joints for signs of swelling or tenderness. He or she will also ask about your symptoms and past health.
You may have blood tests, X-rays, and other tests to find out if another problem is causing your joint pain.
How is it treated?
Treatment for rheumatoid arthritis continues throughout your life. It includes medicine, exercise, and lifestyle changes. Getting treatment early may control the condition or keep it from getting worse.
Many of the medicines used to treat rheumatoid arthritis have side effects. So it is important to have regular checkups and talk with your doctor about any problems. This will help your doctor find a treatment that works for you.
At home, there are things you can do to relieve your symptoms.
- Rest when you are tired.
- Protect your joints from injury by using devices like special kitchen tools or doorknobs.
- Use splints, canes, or walkers to ease pain and take stress off your joints if your symptoms are severe.
- Eat a balanced diet.
- Exercise regularly.
- Stay at a healthy weight.
If you try medicine, exercise, and lifestyle changes for at least a few years but pain and disability get much worse, surgery may be an option. Total joint replacement of the hip and knee are the most successful.
It can be hard to live with a long-term illness that can limit your ability to do things. It is common for people with rheumatoid arthritis to feel depressed. Your mood can affect how you feel and how well you cope with pain. Be sure to seek the help and support you need from friends and family members. Professional counseling can also help.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Cause
The cause of rheumatoid arthritis (RA) is not fully understood. Genes play a role, but experts don’t know exactly what that role is. For most people with RA, the disease doesn’t run in their families and they don’t pass it along to their children. One or more genes may make it more likely that the body’s immune system will attack the tissues of the joints. This immune response may also be triggered by bacteria, a virus, or some other foreign substance.
Other causes of joint pain include osteoarthritis, lupus, and gout.
Symptoms
Joint pain can be an early symptom of many different diseases. In rheumatoid arthritis, symptoms often develop slowly over a period of weeks or months. Fatigue and stiffness are usually early symptoms. Weight loss and a low-grade fever can also occur.
Joint symptoms include:
- Painful, swollen, tender, stiff joints. The same joints on both sides of the body (symmetrical) are usually affected, especially the hands, wrists, elbows, feet, ankles, knees, or neck.
- Morning stiffness. Joint stiffness may develop after long periods of sleeping or sitting. It usually lasts at least 1 hour and often up to several hours.
- Bumps (nodules). Rheumatoid nodules ranging in size from a pea to a mothball develop in nearly one-third of people who have rheumatoid arthritis. Nodules usually form over pressure points in the body such as the elbows, knuckles, spine, and lower leg bones.
In addition to specific joint symptoms, rheumatoid arthritis can cause symptoms throughout the body (systemic). These include:
- Fatigue.
- A loss of appetite.
- Weight loss.
- Mild fever.
Some of the symptoms of rheumatoid arthritis may be similar to symptoms of other health conditions.
More information
What Happens
The course of rheumatoid arthritis is hard to predict. It usually progresses slowly, over months or years. In some people it doesn’t get worse, and symptoms stay about the same. But in rare cases, symptoms come on rapidly, within days.
Symptoms can come and go. You may have times in your life when joint pain goes away on its own for a while. This is called remission.
If the disease progresses, joint pain can restrict simple movements, such as your ability to grip, and daily activities, such as climbing stairs. It is a common cause of permanent disability. But early treatment may control the disease and keep it from getting worse.
Rheumatoid arthritis is more likely to get worse when:
- A rheumatoid factor blood test is positive.
- A blood test for the antibody CCP (cyclic citrullinated peptide) is positive.
- The disease fails to respond to therapy.
- Bumps (nodules) form rapidly.
- Many joints are affected.
- X-rays show early loss of bone or cartilage.
Joint damage
The ongoing inflammation caused by rheumatoid arthritis affects the tissues that line joints. It causes a breakdown in cartilage and loosens ligaments and tendons that support the joints. The resulting joint destruction can lead to deformed joints.
The pain, stiffness, fatigue, and whole-body (systemic) symptoms of rheumatoid arthritis can be disabling. Over time, the deformity caused by the disease can lead to difficulty with daily activities. Specific joint problems may also occur later in the course of the disease.
The hands and wrists and feet may be deformed. The hands are the most common location for deformities.
Inflammation of the knees, if not controlled by treatment, can cause erosion of cartilage and can later lead to the need for knee replacement surgery.
Rheumatoid arthritis can also damage the cervical spine, or neck. This damage can limit how easily you can move your neck. In rare cases, the damage can pinch a nerve or affect the spinal cord and cause numbness, pain, weakness, or paralysis in the arms or legs.
Other problems
In a small number of severe cases, the disease may damage other organs, such as the eyes and lungs.
People who have rheumatoid arthritis seem to develop plaque deposits in arteries (atherosclerosis) earlier than people who do not have rheumatoid arthritis. Inflammation may play a role in speeding up plaque development. When plaque develops in the arteries in the heart, it is called coronary artery disease (CAD) and it increases the risk of a heart attack. When plaque develops in the arteries in the neck, it increases the risk of stroke.
Rheumatoid arthritis and some of the medicines used to treat it can increase the risk of osteoporosis.
It is common for people with rheumatoid arthritis to feel depressed. These feelings may be caused by pain and progressive disability.
Most women with rheumatoid arthritis can become pregnant and have a healthy baby.
What Increases Your Risk
Things that may increase your risk for rheumatoid arthritis include:
- Being female. Rheumatoid arthritis affects women 2 to 3 times as often as men.
- Being middle-aged. Rheumatoid arthritis can begin at any age, but it most often begins in adulthood.
- Smoking cigarettes.
When to Call a Doctor
Call your doctor immediately if you have:
- Sudden, unexplained swelling and pain in any joint or joints.
- Joint pain associated with a fever or rash.
- Pain that is so severe that you cannot use the joint.
- Back or neck pain along with weakness in your arms or legs.
- Loss of bowel or bladder control.
Call your doctor within the next few days if you have:
- Joint pain that continues and has not improved for over 6 weeks.
- Side effects that occur with large doses of nonsteroidal anti-inflammatory drugs (NSAIDs) or other medicine used to treat your arthritis. NSAIDs include ibuprofen (Advil) and naproxen (Aleve).
Watchful waiting
Watchful waiting is a wait-and-see approach. It is reasonable to try home treatment for mild joint pain and stiffness. If there is no improvement after 6 weeks, or if any other symptoms are present, call your doctor.
Early treatment can slow and sometimes prevent significant joint damage. So if you have symptoms similar to rheumatoid arthritis, see your doctor to find out if you have rheumatoid arthritis. Early diagnosis and treatment allows for possible reduction of joint pain, slows joint destruction, and reduces the chance of permanent disability.
Who to see
Early arthritis symptoms can be diagnosed by:
- A nurse practitioner.
- A physician assistant.
- A family medicine doctor.
- An internist.
- A rheumatologist.
Rheumatoid arthritis can be treated by:
- A rheumatologist.
- A family medicine doctor or an internist who consults with a rheumatologist.
Supportive treatment can be provided by:
- An orthopedic surgeon, if surgery is needed.
- A physical therapist.
- An occupational therapist.
- Getting counseling.
Exams and Tests
No single lab test can diagnose rheumatoid arthritis. Instead, doctors look at symptoms and physical signs and then rule out other diseases that can cause similar symptoms.
A medical history and physical exam are usually done to help find the cause of joint pain. The pattern and nature of joint symptoms are the most important clues to the diagnosis.
Diagnosis is based on a set of classification criteria. The criteria include the results of these tests:
- Anti-cyclic citrullinated peptide antibody (ACPA or anti-CCP) test (helps confirm diagnosis and may show your risk of having severe symptoms)
- C-reactive protein (may help to assess disease activity)
- Erythrocyte sedimentation rate (may help to assess disease activity)
- Rheumatoid factor
Other tests are used to help monitor and manage rheumatoid arthritis. These include:
- Antinuclear antibody assay.
- Bone density test, to check for bone loss (osteoporosis).
- Complete blood count.
- Eye exam.
- Imaging tests such as magnetic resonance imaging (MRI), ultrasound, or X-rays.
- Joint fluid analysis.
- Kidney function tests.
- Liver and muscle enzyme tests.
- Tissue type test.
Regular checkups
Because rheumatoid arthritis can lead to severe joint destruction and disability over time, regular checkups are important to see if treatment is working or needs to be adjusted.
Treatment Overview
Rheumatoid arthritis is most often treated with medicine, exercise, and lifestyle changes. Treatment may help relieve symptoms and control the disease, but there is no cure. Treatment for rheumatoid arthritis usually continues throughout your life, but it will vary depending on:
- The stage (active or in remission) and severity of your disease.
- Your treatment history.
- The benefits and risks of treatment options.
- Your preferences for treatment options, such as cost, side effects, and daily schedules.
The goal of treatment is to help you maintain your lifestyle, reduce joint pain, slow joint damage, and prevent disability.
Making a plan
Treatment of rheumatoid arthritis should start with education about the disease, the possibility of joint damage and disability, and the risks and benefits of potential treatments. A long-term treatment plan should be developed by you and your team of doctors.
Treatment with medicines
Early and ongoing treatment of RA with medicines called disease-modifying antirheumatic drugs (DMARDs) can slow or sometimes prevent joint destruction. Other medicines may be combined with DMARDs to relieve symptoms. These medicines include:
- Medicines that reduce swelling, including ibuprofen (such as Advil or Motrin) and naproxen (such as Aleve or Naprosyn).
- Medicines that relieve pain, such as acetaminophen, codeine, and hydrocodone.
- Corticosteroids for early treatment, to control flare-ups, or to help manage the disease.
Be safe with medicines. Read and follow all instructions on the label.
For more information, see Medications.
Lifelong care
Treatment for rheumatoid arthritis usually continues throughout your life. Your doctor will want to closely monitor your condition. A rheumatologist should evaluate you regularly. Depending on your symptoms and treatment, this could be done as often as every 2 to 3 months or every 6 to 12 months. Testing, such as blood tests, may be done more often.
During each follow-up visit, your doctor will assess:
- The amount of joint pain.
- How long morning stiffness lasts.
- The number of actively inflamed joints.
- How well you are functioning.
- Results of lab tests.
In some cases, the disease does not respond to the first several treatments. When this happens, the disease may be treated with much higher doses of medicines or with different combinations of medicines.
Surgery may be considered when the joints—especially the hips, knees, or feet—are severely damaged or deformed and are causing extreme pain. Surgery may include total joint replacement or other techniques to improve joint function. For more information, see Surgery and Other Treatment.
Exercise and lifestyle changes
Exercise, physical therapy, and lifestyle changes can help relieve joint pain. Many people with RA benefit from self-care plans that balance rest and activity. You can take steps at home to relieve your symptoms and help control your disease. For more information, see Living With Rheumatoid Arthritis.
Living With Rheumatoid Arthritis
Living with rheumatoid arthritis often means making changes to your lifestyle. You can do things at home, such as staying active and taking medicines, to help relieve your symptoms and prevent the disease from getting worse.
You can also plan for those times when the disease symptoms may be more severe. It is important to work closely with your health professionals, who may include a physical therapist or counselor, to find ways to reduce pain.
Rest when you’re tired
The disease itself causes fatigue. And the strain of dealing with pain and limited activities also can make you tired. The amount of rest you need depends on how bad your symptoms are.
- With severe symptoms, you may need long periods of rest. You might need to rest a joint by lying down for 15 minutes several times a day to relax. Try to find a balance between daily activities that you must do or want to do and the amount of rest you need to do those activities.
- Plan your day carefully, including rest periods. Pace your activities so that you don’t get overtired.
Protect your joints
You may need to change the way you do certain activities so that you are not overusing your joints. Try to find different ways to relieve your joint pain.
- Joint pain and stiffness may improve with heat therapy, such as:
- Taking warm showers or baths after long periods of sitting or sleeping.
- Soaking hand joints in warm wax baths.
- Sleeping under a warm electric blanket.
- Use assistive devices to reduce strain on your joints, such as special kitchen tools or doorknobs.
- Choose the right shoes that fit well and will not cause joint problems.
- Use splints, canes, or walkers to reduce pain and improve function.
Stay active
Keep moving to keep your muscle strength, flexibility, and overall health.
- Physical therapy may be recommended by your doctor.
- Exercise for arthritis takes three forms—stretching, strengthening, and conditioning. Exercise can improve or maintain quality of life for people who have rheumatoid arthritis. Your specific joint problem may guide the type of activity that will help the most. For example:
- Swimming is a good activity if you have joint problems in your knees, ankles, or feet.
- Bicycling and walking are good activities if your joint problems are not in your legs or feet.
Avoid smoking
People with rheumatoid arthritis have an increased risk of plaque in the arteries (atherosclerosis). Smoking increases this risk even more. Smoking may also lower your response to treatment.footnote 1 So, if you’re a smoker, quit. For more information on how to quit, see the topic Quitting Smoking.
Eat healthy foods
Try to eat a variety of healthy foods. Dietary needs are not the same for all people who have rheumatoid arthritis. To be sure you get the nutrients you need, you can ask a registered dietitian to help you make a plan.
- Be sure to get enough calcium and vitamin D to protect your bones against osteoporosis. For more information, see the topic Osteoporosis.
- Lose weight, if you are overweight. For more information, see the topic Weight Management.
- People who have rheumatoid arthritis also have an increased risk of heart disease. But healthy lifestyle changes, such as exercise and a healthy diet, may reduce your risk.
For more information, see:
Take care of your teeth and gums
People who have rheumatoid arthritis tend to get gum disease. Some experts think that infection that enters the body through the mouth may make rheumatoid arthritis worse, although this has not been proved. You can help prevent gum disease through good basic dental care.
Medications
Medicines are the main treatment for rheumatoid arthritis. The types of medicines used depend on how severe your disease is, how fast it is progressing, and how it affects your daily life.
If your symptoms ease, you and your doctor will decide if you can take less medicine or stop taking medicine. If your symptoms get worse, you will have to start taking medicine again.
Medicines are used to:
- Relieve or reduce pain.
- Improve daily function.
- Reduce joint inflammation. Signs of joint inflammation include swelling, tenderness, and limited range of motion.
- Prevent or delay significant joint damage and deformity.
- Prevent permanent disability.
- Improve quality of life.
Medicines called disease-modifying antirheumatic drugs (DMARDs) can slow or sometimes prevent joint destruction. Starting treatment early with DMARDs can reduce the severity of the disease. DMARDs are also called immunosuppressive drugs or slow-acting antirheumatic drugs (SAARDs). These medicines are usually taken over a long period to help control the disease.
DMARDs can be thought of as nonbiologic or biologic, depending on how they are made and how they act in the body. But they are all used to block harmful responses from the body’s immune system. DMARDs are sometimes combined with one another or with other medicines. By combining medicines, you may be able to take lower doses of individual medicines. This may reduce your risk of side effects.
Some medicines for rheumatoid arthritis may cause birth defects. If you are pregnant or are trying to become pregnant, talk with your doctor about your medicines.
Medicines to slow the disease
Disease-modifying antirheumatic drugs (DMARDs) are usually started within 3 months of your diagnosis. They are used to control the progression of RA and to try to prevent joint damage and disability. DMARDs are often given in combination with other medicines.
Commonly used nonbiologic DMARDs
- Antimalarials such as hydroxychloroquine or chloroquine
- Leflunomide
- Methotrexate
- Sulfasalazine
Less commonly used nonbiologic DMARDs
- Azathioprine
- Cyclophosphamide
- Cyclosporine
- Gold salts
- Minocycline
- Penicillamine
Biologic DMARDs (biologics)
- Abatacept
- Adalimumab
- Anakinra
- Certolizumab
- Etanercept
- Golimumab
- Infliximab
- Rituximab
- Tocilizumab
There is a newer biologic drug called tofacitinib (Xeljanz) for adults who have moderate to severe rheumatoid arthritis. This medicine is for people who have not responded well to methotrexate or who cannot take it. Tofacitinib is taken by mouth. It reduces the symptoms of rheumatoid arthritis and allows people to be more active. But the long-term safety of this medicine is still being studied.footnote 2, footnote 3
Medicines to relieve symptoms
- Nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen, and naproxen. NSAIDs are used to control pain and may help reduce inflammation. They don’t control the disease or stop it from getting worse. NSAIDs may be combined with DMARDs.
- Corticosteroids such as prednisone. These medicines are used to reduce disease activity and joint inflammation. But using only corticosteroids for an extended time is not considered the best treatment. Corticosteroids are often used to control symptoms and flares of joint inflammation until DMARDs reach their full effectiveness.
- Analgesics (pain relievers). These don’t reduce inflammation but may help with pain control. They include:
- Nonprescription acetaminophen.
- Acetaminophen with codeine (such as Tylenol with codeine).
- Acetaminophen with hydrocodone (such as Vicodin).
- Tramadol.
What to think about
- Some DMARDs can take up to 6 months to work.
- In some people, a certain DMARD may not work at all. So a different DMARD will be used.
- If you’re taking DMARDs, it’s a good idea to have a rheumatologist manage your care.
- Many DMARDs have serious side effects. You will need regular blood and urine tests to check the drug’s effects on blood-producing cells (bone marrow), the kidneys, and the liver.
- If you have other conditions such as high blood pressure or high cholesterol, your doctor may recommend that you take medicine to control them.
Be safe with medicines. Read and follow all instructions on the label.
Surgery
Surgical treatment for rheumatoid arthritis is used to relieve severe pain and improve function of severely deformed joints that don’t respond to medicine and physical therapy.
Total joint replacement (arthroplasty) can be done for many different joints in the body. Its success varies depending on which joint is replaced.
Surgery choices
Surgeries considered for people who have severe rheumatoid arthritis include:
- Arthroplasty, to replace part or all of a joint, such as the hip or knee.
- Arthroscopy, which uses a small lighted instrument to remove debris or inflamed tissue from a joint.
- Carpal tunnel release, to relieve pressure on the median nerve in the wrist.
- Cervical spinal fusion, to treat severe neck pain and nerve problems.
- Finger and hand surgeries, to correct joint problems in the hand.
- Foot surgery such as phalangeal head resection.
- Synovectomy, to remove inflamed joint tissue.
What to think about
Joint surgery often restores near-normal movement in a person who has osteoarthritis in just one or two joints. But this is not the case for people affected by rheumatoid arthritis.
- Rheumatoid arthritis usually affects multiple joints, particularly smaller joints, such as finger joints, which are needed for many daily activities. Surgical treatment may not be an option for all of the affected joints.
- Joint surgery or replacement can relieve disabling pain and restore enough motion to allow you to do your daily activities. But it will seldom restore the joint to normal.
Before you decide to have surgery, consult with an orthopedic surgeon who is experienced in joint surgery for rheumatoid arthritis.
Other Treatment
Other types of treatment that may help you control some of the symptoms of rheumatoid arthritis include:
- Physical therapy, to improve joint function. Physical therapy includes exercise, hot and cold therapy, and massage.
- Occupational therapy. This helps you learn how to maintain movement in the joints while carrying out the activities of daily living.
- Assistive devices such as household aids or mobility aids. For more information and a catalog, contact the Arthritis Foundation at www.arthritis.org.
- Behavioral modification techniques to reduce pain and stress. These include biofeedback and relaxation therapy, such as breathing exercises and muscle relaxation.
- Counseling. It can help you cope with long-term pain and disability.
Complementary medicine
Complementary medicine therapies are used by many people to relieve symptoms and improve their quality of life, even though there isn’t strong scientific evidence that they help. These therapies include:
- Acupuncture. This treatment is used to relieve pain and treat certain health conditions. It is done by inserting very thin needles into the skin at specific points on the body.
- Herbs and dietary supplements. If you decide to use herbs or dietary supplements, be sure to tell your doctor.
- Herbs such as the oil of evening primrose, borage seed, or blackcurrant seed may help relieve symptoms and improve function without significant side effects.
- Essential fatty acids (such as fish oil) may provide some relief of symptoms.footnote 4
- The dietary supplements glucosamine and chondroitin are sometimes used to try to relieve joint pain. But there is not evidence that they are effective for rheumatoid arthritis.
- Massage. It can help relieve stress and reduce pain. But don’t massage swollen or painful joints.
Find out about the safety of any complementary product or practice you want to try. Most mind and body practices—such as acupuncture and massage—are safe when used under the care of a well-trained professional. Choose an instructor or practitioner as carefully as you would choose a doctor.
Talk with your doctor about any complementary health practice that you would like to try or are already using. Your doctor can help you manage your health better if he or she knows about all of your health practices.
References
Citations
- O’Dell JR (2013). Treatment of rheumatoid arthritis. In GS Firestein et al., eds., Kelley’s Textbook of Rheumatology, 9th ed., vol. 2, pp. 1137–1160. Philadelphia: Saunders.
- Fleischmann R, et al. (2012). Placebo-controlled trial of tofacitinib monotherapy in rheumatoid arthritis. New England Journal of Medicine, 367(6): 495–507.
- Von Vollenhoven RF, et al. (2012). Tofacitinib or adalimumab versus placebo in rheumatoid arthritis. New England Journal of Medicine, 367(6): 508–519.
- Gomez FE, Kaufer-Horwitz M (2012). Medical nutrition therapy for rheumatic disease. In LK Mahan et al., eds., Krause’s Food and the Nutrition Care Process, 13th ed., pp. 901–922. St Louis: Saunders.
Other Works Consulted
- O’Dell JR (2013). Treatment of rheumatoid arthritis. In GS Firestein et al., eds., Kelley’s Textbook of Rheumatology, 9th ed., vol. 2, pp. 1137–1160. Philadelphia: Saunders.
- Singh JA, et al. (2016). 2015 American College of Rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Care and Research, 68(1): 1–25. DOI: 10.1002/acr.22783. Accessed April 14, 2016.
- Steultjens EEMJ, et al. (2009). Occupational therapy for rheumatoid arthritis. Cochrane Database of Systematic Reviews (1).
- Sweeney SE, et al. (2013). Clinical features of rheumatoid arthritis. In GS Firestein et al., eds., Kelley’s Textbook of Rheumatology, 9th ed., vol. 2, pp. 1109–1136. Philadelphia: Saunders.
- Yasuda GT, et al. (2013). Rheumatoid arthritis. In JE Pizzorno, MT Murray, eds., Textbook of Natural Medicine, 4th ed., pp. 1769–1784. St. Louis: Elsevier.
Credits
Current as ofApril 1, 2019
Author: Healthwise Staff
Medical Review: Anne C. Poinier, MD – Internal Medicine
E. Gregory Thompson, MD – Internal Medicine
Adam Husney, MD – Family Medicine
Martin J. Gabica, MD – Family Medicine
Kathleen Romito, MD – Family Medicine
Nancy Ann Shadick, MD, MPH – Rheumatology
Current as of: April 1, 2019
Author: Healthwise Staff
Medical Review:Anne C. Poinier, MD – Internal Medicine & E. Gregory Thompson, MD – Internal Medicine & Adam Husney, MD – Family Medicine & Martin J. Gabica, MD – Family Medicine & Kathleen Romito, MD – Family Medicine & Nancy Ann Shadick, MD, MPH – Rheumatology
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.