Ringworm of the Scalp or Beard
Topic Overview
Is this topic for you?
This topic is about ringworm of the scalp or beard. To learn more about other fungal infections, see the topics:
What is ringworm of the scalp or beard?
Ringworm is an infection on your skin, hair, or nails. It’s caused by a fungus. The medical term for fungal infections is tinea, followed by a word that describes the location of infection. So ringworm of the scalp is tinea capitis, and ringworm of the beard is tinea barbae.
Ringworm of the scalp occurs all over the world and is most common in young children. Ringworm of the beard is not common.
What causes ringworm of the scalp or beard?
Ringworm is caused by a fungus, not by a worm. The kinds of fungi (plural of fungus) that cause ringworm live and spread on the top layer of the skin and on the hair.
Ringworm is contagious. You can catch it by touching a person or animal that has it or by sharing personal items such as hats, combs, brushes, towels, and clothing. The fungi can survive for several months on people, animals, and personal items.
Children are more likely to get ringworm than adults. When adults do get infected, they often become carriers. This means they don’t have symptoms but can pass ringworm to others.
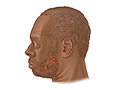
What does ringworm of the scalp or beard look like?
Ringworm of the scalp or beard often looks like round, bald patches. In most cases, the infection spreads outward while the inside of the circle clears up. This makes the infection look like a ring. That’s why it’s called “ringworm.”
But ringworm doesn’t always make a ring pattern. Sometimes it looks like:
- Dandruff.
- Patches of black dots, which are the stubble of hair that’s broken off at the scalp.
- Red, crusty, swollen areas with small bumps that look like blisters.
Ringworm spreads easily from one person to another. If anyone in your family has the symptoms listed above, see your doctor.
How is ringworm of the scalp or beard diagnosed?
Your doctor may be able to diagnose ringworm just by how the rash looks. To check for the ringworm fungus, your doctor may look at a hair or skin sample under a microscope. This test is called a KOH preparation.
If it’s not clear that you have ringworm, or if the treatment isn’t working, your doctor may do a skin culture to find out what kind of germ is causing the problem.
How is it treated?
Your doctor will prescribe pills that will kill the fungus. And you can use special shampoo that may keep ringworm from spreading to others. But you need to use the shampoo along with the pills. By itself, the shampoo can’t completely destroy the fungi causing the infection.
Depending on the medicine you take:
- Your doctor may want to check your blood work during treatment. These tests are to make sure that the medicine isn’t affecting your blood counts or your liver or kidney function.
- You may need to take antifungal pills for as few as 4 weeks or as long as 12 weeks. Be sure to take the full course of your medicine.
If you treat ringworm early, the hair in the bald spots will probably grow back. If you don’t treat it, the bald spots could be permanent.
If your child gets ringworm, ask the school nurse or local health department how long your child needs to stay out of school. Usually children can go to school after they have started treatment with antifungal medicine. You don’t need to shave your child’s head.
How can you keep ringworm from coming back?
Ringworm of the scalp or beard can come back after treatment has cleared the infection. To help prevent it from coming back:
- Throw away your combs and brushes and buy new ones as soon as you start treatment.
- Wash your hair or beard once a month with a shampoo that contains selenium sulfide (such as Selsun Blue or Head and Shoulders Intensive Treatment).
- Don’t share hats, combs, brushes, or towels with others.
- Wash your clothes, towels, and bed sheets in hot water.
- Keep your skin clean and dry.
References
Other Works Consulted
- Elewski BE, et al. (2008). Terbinafine hydrochloride oral granules versus oral griseofulvin suspension in children with tinea capitis: Results of two randomized, investigator-blinded, multicenter, international, controlled trials. Journal of the American Academy of Dermatology, 59(1): 41–54.
- Grossberg R (2015). Fungal diseases of the skin. In ET Bope et al., eds., Conn’s Current Therapy 2015, pp. 261–262. Philadelphia: Saunders.
- Habif TP, et al. (2011). Tinea of the beard (tinea barbae). In Skin Disease: Diagnosis and Treatment, 3rd ed., pp. 288–289. Edinburgh: Saunders.
- Habif TP, et al. (2011). Tinea of the scalp (tinea capitis). In Skin Disease: Diagnosis and Treatment, 3rd ed., pp. 284–287. Edinburgh: Saunders.
- Higgins EM (2010). Tinea capitis. In MG Lebwohl et al., eds., Treatment of Skin Disease: Comprehensive Therapeutic Strategies, 3rd ed., pp. 736–739. Edinburgh: Saunders Elsevier.
Current as of: April 1, 2019
Author: Healthwise Staff
Medical Review:Kathleen Romito, MD – Family Medicine & Adam Husney, MD – Family Medicine & Martin J. Gabica, MD – Family Medicine
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.