Sudden Infant Death Syndrome (SIDS)
Topic Overview
What is sudden infant death syndrome (SIDS)?
Sometimes a baby who seems healthy dies during sleep. This is called sudden infant death syndrome or SIDS.
In most cases, a parent or caregiver places the baby down to sleep and returns later to find the baby has died. It’s no one’s fault. SIDS can happen even when you do everything right.
Although SIDS is rare, it is one of the most common causes of death in babies between 1 and 12 months of age. Most babies who die of SIDS are between the ages of 2 and 4 months.
What causes SIDS?
Doctors don’t know what causes SIDS. It seems to happen more often in premature and low-birth-weight babies. It also is seen more often in babies whose mothers didn’t get medical care during the pregnancy and in babies whose mothers smoke. SIDS may also be more likely in babies who were part of a multiple pregnancy (for example, twins or triplets) or whose mothers are younger than 20.
When babies sleep on their bellies, they may not breathe well. Not too long ago, side sleeping was said to be okay. But babies placed on their sides can easily roll onto their bellies and could have trouble breathing.
Researchers are studying the possibility that SIDS may be caused by problems with how well the brain controls breathing, heart rate and rhythm, and temperature during the first few months of life. More research on this is needed.
What are the symptoms?
SIDS has no symptoms or warning signs. Babies who die of SIDS seem healthy before being put to bed. They show no signs of struggle and are often found in the same position as when they were placed in the bed.
How is SIDS diagnosed?
SIDS is named the cause of death only when no other cause is found. To find out why a baby died, medical experts review the baby’s and parents’ medical histories, study the area where the baby died, and do an autopsy.
What can you do to reduce the risk of SIDS?
Doing certain things may help protect a baby from SIDS and/or other deaths related to sleep:footnote 1
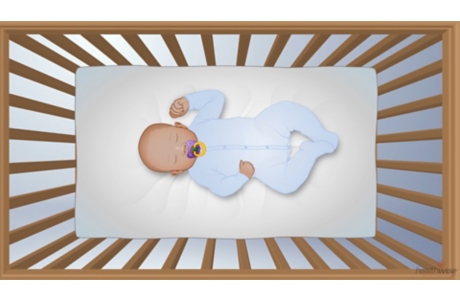
- The most important thing you can do is toalways place your baby to sleep on his or her backrather than on the stomach or side.
- Don’t use tobacco, alcohol, or drugs while you are pregnant. And don’t expose your baby to secondhand smoke during or after your pregnancy.
- For the first 6 months, have your baby sleep in a crib, cradle, or bassinet in the same room where you sleep. The American Academy of Pediatrics recommends that you don’t ever sleep with your baby in the same bed, especially if you smoke or have used alcohol, illegal drugs, or medicine that makes you sleep very soundly (sedatives).
- Never sleep with a baby on a couch or armchair. And it is not safe to place your baby on a couch to sleep. It is not safe to place your baby in a car seat, sling, swing, bouncer, or stroller to sleep. The safest place for a baby is in a crib, cradle, or bassinet that meets safety standards.
- Keep soft items and loose bedding out of the crib. Items such as blankets, stuffed animals, toys, and pillows could suffocate or trap your baby. Dress your baby in sleepers instead of using blankets.
- Make sure that your baby’s crib has a firm mattress (with a fitted sheet). Don’t use bumper pads or other products that attach to crib slats or sides. They could suffocate or trap your baby.
- Never use a sleep positioner. Using a sleep positioner to hold a baby on his or her side or back can be dangerous.
- Keep the room at a comfortable temperature so that your baby can sleep in lightweight clothes without a blanket. Usually, the temperature is about right if an adult can wear a long-sleeved T-shirt and pants without feeling cold. Make sure that your baby doesn’t get too warm. Your baby is likely too warm if he or she sweats or tosses and turns a lot.
- Breastfeed your baby and have your baby immunized.
- Consider giving your baby a pacifier at nap time and bedtime. This may help prevent SIDS, though experts don’t know why. If you breastfeed, wait until your baby is about a month old before you start giving him or her a pacifier.
There is no sure way to prevent SIDS, and no exam or test can predict whether a baby is likely to die of SIDS. Don’t rely on breathing (apnea) monitors, special mattresses, or other devices marketed as a way to reduce your baby’s risk of SIDS. None of these items have been proved to lower the risk of SIDS. The American Academy of Pediatrics does not advise their use.
Remember, SIDS is rare. Be as safe as you can, but don’t let fear keep you from enjoying your baby. Tell your baby’s caregivers what you expect them to do. Don’t assume that they know what to do to help keep your infant safe during sleep.
How can a family cope after losing a baby to SIDS?
Each member of your family may respond to the loss of the baby in a different way. These different ways of coping with the baby’s death can strain a marriage and a family. Along with feeling grief, family members may be struggling with feelings of guilt. Support from family, friends, your doctor, and possibly other health professionals is very important for everyone. You might find it helpful to:
- Join a grief support group. Ask your doctor if one for parents who have lost babies to SIDS is available in your area.
- Get help from a counselor, a psychologist, or a psychiatrist. Many families benefit from group counseling to help them deal with the tensions that arise after the loss of a baby.
- Talk with a close family member, a friend, or a spiritual adviser.
References
Citations
- Task Force on Sudden Infant Death Syndrome (2016). SIDS and other sleep-related infant deaths: Updated 2016 recommendations for a safe infant sleeping environment. Pediatrics, 138(5): e20162938. DOI: 10.1542/peds.2016-2938. Accessed October 24, 2016.
Other Works Consulted
- Academy of Breastfeeding Medicine Protocol Committee (2008). ABM clinical protocol #6: Guideline on co-sleeping and breastfeeding. Breastfeeding Medicine, 3(1): 38–43.
- Corwin MJ (2011). Apparent life-threatening events and SIDS. In CD Rudolph et al., eds., Rudolph’s Pediatrics, 22nd ed., pp. 451–454. New York: McGraw-Hill.
- Federico M, et al. (2014). Respiratory tract and mediastinum. In WW Hay Jr et al., eds., Current Diagnosis and Treatment: Pediatrics, 22nd ed., pp. 534–587. New York: McGraw-Hill.
- Hauck FR, Tanabe KO (2009). SIDS, search date April 2007. Online version of BMJ Clinical Evidence. Also available online: http://www.clinicalevidence.com.
- Hunt CE, Hauck FR (2011). Sudden infant death syndrome. In RM Kliegman et al., eds., Nelson Textbook of Pediatrics, 19th ed., pp. 1421–1429. Philadelphia: Saunders.
- Hymel KP and the Committee on Child Abuse and Neglect, American Academy of Pediatrics (2006, reaffirmed 2009). Clinical report: Distinguishing sudden infant death syndrome from child abuse fatalities. Pediatrics, 118(1): 421–427.
- Kline A, Gibson E (2006). Sudden infant death syndrome. In FD Burg et al., eds., Current Pediatric Therapy, 18th ed., pp. 258–260. Philadelphia: Saunders Elsevier.
- Rechtman L, et al. (2014). Sofas and infant mortality. Pediatrics, 134(5): e1293. DOI: 10.1542/peds.2014-1543. Accessed October 31, 2014.
Current as of: December 12, 2018
Author: Healthwise Staff
Medical Review:John Pope, MD, MPH – Pediatrics & Kathleen Romito, MD – Family Medicine & Susan C. Kim, MD – Pediatrics
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.