Gastroesophageal Reflux in Babies and Children
Topic Overview
What is gastroesophageal reflux?
Gastroesophageal reflux happens when food and stomach acid flow from the stomach back into the esophagus. The esophagus is the tube that carries food from the mouth to the stomach. In adults, reflux is often called heartburn or acid reflux.
Reflux is common in babies and children, and it is usually not a sign of a serious problem. Most babies stop having reflux around 1 year of age. A child who continues to have reflux may need treatment.
What causes reflux?
Reflux happens because of a problem with the ring of muscle at the end of the esophagus. The ring of muscle is called the lower esophageal sphincter, or LES. The LES acts like a one-way valve between the esophagus and the stomach. When you swallow, it lets food pass into the stomach. If the LES is weak, stomach contents can flow back up into the esophagus.
In babies, this problem happens because the digestive tract is still growing. Reflux usually goes away as a baby matures.
What are the symptoms?
It is common for babies to spit up (have reflux) after they eat. Babies with severe reflux may cry, act fussy, or have trouble eating. They may not sleep well or grow as expected.
An older child or teen may have the same symptoms as an adult. He or she may cough a lot and have a burning feeling in the chest and throat (heartburn). He or she may have a sour or bitter taste in the mouth.
If stomach acid goes up to the throat or into the airways, a child may get hoarse or have a lasting cough. Reflux can also cause pneumonia or wheezing, and it may hurt to swallow.
How is reflux diagnosed?
To find out if a child has reflux, a doctor will do a physical exam and ask about symptoms. A baby who is healthy and growing may not need any tests. If a teen is having symptoms, the doctor may want to see if medicines help before doing tests.
If a baby is not growing as expected or treatment doesn’t help a teen, the doctor may want to do tests to help find the cause of the problem. Common tests include:
- A barium swallow, which is a series of X-rays that shows the esophagus and stomach.
- Endoscopy, which lets the doctor look at the esophagus.
- An esophageal pH test, which measures how much acid is in the esophagus.
How is it treated?
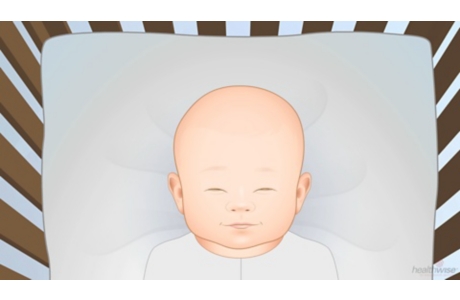
Most babies stop having reflux over time, so the doctor may just suggest that you follow some steps to help reduce the problem until it goes away. For example, it may help to:
- Burp your baby a few times during each feeding.
- Keep your baby upright for 30 minutes after each feeding. Avoid a “car seat position,” because sitting can make reflux worse in babies.
- Avoid feeding too much at one time. Give your baby smaller meals more often.
- Thicken your baby’s formula with a small amount of rice cereal if your doctor recommends it.
- Keep your baby away from smoky areas.
For older children and teens, it may help to:
- Avoid large meals before exercise.
- Raise the head of your child’s bed 6 in. (15 cm) to 8 in. (20 cm). Using extra pillows does not work.
- Have your child stay upright for 2 to 3 hours after eating.
- Serve 5 or 6 small meals instead of 2 or 3 big ones.
- Limit foods that might make reflux worse. These include chocolate, sodas that have caffeine, spicy foods, fried foods, and high-acid foods such as oranges and tomatoes.
- Keep your child away from smoky areas.
If these steps don’t work, the doctor may suggest medicine. Medicines that may be used include:
- Antacids, such as Mylanta and Maalox. Antacids neutralize stomach acid and relieve heartburn. You can buy these without a prescription. But they are not usually recommended for long-term use. Be careful when you give your child over-the-counter antacid medicines. Many of these medicines have aspirin in them. Do not give aspirin to anyone younger than 20. It has been linked to Reye syndrome, a serious illness.
- Acid reducers that decrease the amount of acid the stomach makes.
- H2 blockers, such as cimetidine (Tagamet), famotidine (Pepcid), nizatidine (Axid), and ranitidine (Zantac). H2 blockers reduce the amount of acid in the stomach. You can buy some of these without a prescription. For stronger doses, you will need a prescription.
- Proton pump inhibitors, such as esomeprazole (Nexium), lansoprazole (Prevacid), and omeprazole (Prilosec). You can buy some proton pump inhibitors without a prescription.
Before you give your child any over-the-counter medicine for reflux:
- Talk to your child’s doctor.
- Read the label. Do not give a child any product that contains bismuth subsalicylate, such as Pepto-Bismol or Kaopectate. Experts think it may be linked to Reye syndrome, a rare but serious illness.
- Be sure you understand how much and how often to give the medicine to your child. If you are not sure, ask your doctor.
Children with reflux rarely need surgery. It may be an option for babies or children who have severe reflux that causes breathing problems or keeps them from growing.
References
Other Works Consulted
- Hoffenberg E, et al. (2014). Gastrointestinal tract. In WW Hay Jr et al., eds., Current Diagnosis and Treatment: Pediatrics, 22nd ed., pp. 651–691. New York: McGraw-Hill.
- Horvath A, et al. (2008). The effect of thickened-feed interventions on gastroesophageal reflux in infants: Systematic review and meta-analysis of randomized, controlled trials. Pediatrics, 122(6): e1268–e1277.
- Khan S, Orenstein SR (2011). Gastroesophageal reflux disease. In RM Kliegman et al., eds., Nelson Textbook of Pediatrics, 19th ed., pp. 1266–1270. Philadelphia: Saunders.
- Orenstein SR, et al. (2009). Multicenter, double-blind, randomized, placebo-controlled trial assessing the efficacy and safety of proton pump inhibitor lansoprazole in infants with symptoms of gastroesophageal reflux disease. Journal of Pediatrics, 154(4): 514–520.
Current as of: November 7, 2018
Author: Healthwise Staff
Medical Review:John Pope, MD, MPH – Pediatrics & Adam Husney, MD – Family Medicine & E. Gregory Thompson, MD – Internal Medicine & Kathleen Romito, MD – Family Medicine & Arvydas D. Vanagunas, MD, FACP, FACG – Gastroenterology
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.