Lumbar Herniated Disc
Topic Overview
Is this topic for you?
This topic is for a people who have a herniated disc in the lower back. If you are looking for information on a herniated disc in the neck, see the topic Cervical Disc Herniation.

What is a herniated disc?
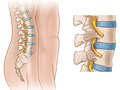
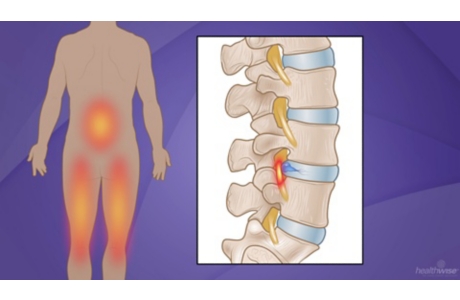
The bones (vertebrae) that form the spine in your back are cushioned by small, spongy discs. When these discs are healthy, they act as shock absorbers for the spine and keep the spine flexible. But when a disc is damaged, it may bulge or break open. This is called a herniated disc. It may also be called a slipped or ruptured disc.
You can have a herniated disc in any part of your spine. But most herniated discs affect the lower back (lumbar spine). Some happen in the neck (cervical spine) and, more rarely, in the upper back (thoracic spine).
What causes a herniated disc?
A herniated disc may be caused by:
- Wear and tear of the disc. As you age, your discs dry out and aren’t as flexible.
- Injury to the spine. This may cause tiny tears or cracks in the hard outer layer of the disc. When this happens, the thick gel inside the disc can be forced out through the tears or cracks in the outer layer of the disc. This causes the disc to bulge or break open.
What are the symptoms of herniated disc?
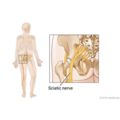
When a herniated disc presses on nerve roots, it can cause pain, numbness, and weakness in the area of the body where the nerve travels. A herniated disc in the lower back can cause pain and numbness in the buttock and down the leg. This is called sciatica (say “sy-AT-ih-kuh”). Sciatica is the most common symptom of a herniated disc in the low back.
If a herniated disc isn’t pressing on a nerve, you may have a backache or no pain at all.
If you have weakness or numbness in both legs along with loss of bladder or bowel control, seek medical care right away. This could be a sign of a rare but serious problem called cauda equina syndrome.
How is a herniated disc diagnosed?
Your doctor may diagnose a herniated disc by asking questions about your symptoms and examining you. If your symptoms clearly point to a herniated disc, you may not need tests.
Sometimes a doctor will do tests such as an MRI or a CT scan to confirm a herniated disc or rule out other health problems.
How is herniated disc treated?
Symptoms from a herniated disc usually get better in a few weeks or months. To help you recover:
- Rest if you have severe pain. Otherwise, stay active. Staying in bed for more than 1 or 2 days can weaken your muscles and make the problem worse. Walking and other light activity may help.
- Try using a heating pad on a low or medium setting for 15 to 20 minutes every 2 or 3 hours. Try a warm shower in place of one session with the heating pad. You can also buy single-use heat wraps that last up to 8 hours. You can also try an ice pack for 10 to 15 minutes every 2 to 3 hours.
- Do the exercises that your doctor or physical therapist suggests. These will help keep your back muscles strong and prevent another injury.
- Ask your doctor about medicine to treat your symptoms. Medicine won’t cure a herniated disc, but it may help with pain and swelling.
Usually a herniated disc will heal on its own over time. Be patient, and keep following your treatment plan. If your symptoms don’t get better in a few months, you may want to talk to your doctor about surgery.
Can a herniated disc be prevented?
After you have hurt your back, you are more likely to have back problems in the future. To help keep your back healthy:
- Protect your back when you lift. For example, lift with your legs, not your back. Don’t bend forward at the waist when you lift. Bend your knees, and squat.
- Use good posture. When you stand or walk, keep your shoulders back and down, your chin back, and your belly in. This will help support your lower back.
- Get regular exercise.
- Stay at a healthy weight. This may reduce the load on your lower back.
- Don’t smoke. Smoking increases the risk of a disc injury.
Frequently Asked Questions
|
Learning about herniated disc: |
|
|
Being diagnosed: |
|
|
Getting treatment: |
|
|
Ongoing concerns: |
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Decision Points focus on key medical care decisions that are important to many health problems.
Actionsets are designed to help people take an active role in managing a health condition.
Cause
Wear and tear, also called disc degeneration, is the usual cause of a herniated disc. As we age, the discs in our back lose some of the fluid that helps them stay flexible. The outer layer of the discs can form tiny tears or cracks. The thick gel inside the disc may be forced out through those cracks and cause the disc to bulge or break open.
This can also happen when you injure your back. Injury can occur from:
- A sudden heavy strain or increased pressure to the lower back. Sometimes a sudden twisting movement or even a sneeze will force some of the material out.
- Activities that are done over and over again that may stress the lower back, including poor lifting habits, prolonged exposure to vibration, and sports-related injuries.
Symptoms
If the herniated disc isn’t pressing on a nerve, you may have an ache in the low back or no symptoms at all.
Only a few people who have herniated discs have severe or troublesome symptoms.
When the disc does press on a nerve, symptoms may include:
- Pain that travels through the buttock and down a leg to the ankle or foot because of pressure on the sciatic nerve. Low back pain may accompany the leg pain.
- Tingling (“pins-and-needles” sensation) or numbness in one leg that can begin in the buttock or behind the knee and extend to the thigh, ankle, or foot.
- Weakness in certain muscles in one or both legs.
- Pain in the front of the thigh.
- Severe deep muscle pain and muscle spasms
Cauda equina syndrome
Weakness in both legs and the loss of bladder and/or bowel control are symptoms of a specific and severe type of nerve root compression called cauda equina syndrome. This is a rare but serious problem. A person with these symptoms should see a doctor right away.
What Happens
Due to age, injury, or both, the outer layer of a spinal disc may dry out and form tiny cracks. Sometimes this causes a:
- Bulging disc.Some of the thick gel in the disc may leak into the cracks. The disc may begin to bulge out from between the bones of the spine (vertebrae).
- Ruptured disc. The gel breaks through the capsule.
- Free fragment. Fragments of a ruptured disc may break completely free of the disc and lodge in the spinal canal.
Any of these stages can cause pressure on a nerve root and symptoms of pain and numbness.
The cracks in the disc don’t repair themselves, but the pain usually fades over time. More than half of the people who have a herniated disc recover in the first 3 months.footnote 1
Long-term problems
It’s important to see your doctor if you’ve had constant or increasing pain for more than 4 to 6 weeks. Getting help early on can lower your chance of having lasting problems, such as the following:
- Pain may come and go. Pain-free periods happen less and less.
- Long-lasting (chronic) and recurring pain can develop because of continued tissue irritation caused by the disc pressing on a nerve.
- Chronic pain syndromecan result from having ongoing pain, causing depression, anxiety, and trouble coping with daily life.
- Symptoms caused by long-term nerve root compression include loss of agility, strength, or sensation in one or both legs and feet.
What Increases Your Risk
Risk factors are things that increase your risk of having a herniated disc. Some risk factors you can change, and some you can’t.
Risk factors that you cannot change
- Getting older.
- Being male.
- Having a history of back injury,previous herniated disc, or back surgery.
Risk factors that you can change
- Your job or other activities.These may include:
- Long periods of sitting.
- Lifting or pulling heavy objects.
- Frequent bending or twisting of the back.
- Heavy physical exertion.
- Repetitive motions.
- Exposure to constant vibration (such as driving).
- Not exercising regularly, doing strenuous exercise for a long time, or starting to exercise too strenuously after a long period of inactivity.
- Smoking. Nicotine and other toxins from smoking can keep spinal discs from absorbing all the nutrients they need from the blood, making disc injury more likely. Smoking also increases your sensitivity to pain.
- Being overweight. Carrying extra body weight (especially in the stomach area) may put additional strain on the lower back, although this hasn’t been proved. But being overweight often also means being in poor physical condition, with weaker muscles and less flexibility. These can lead to low back pain.
When should you call your doctor?
Call 911 or other emergency services immediately if:
- An injury causes numbness or weakness in one or both legs.
Call your doctor now if:
- You have a new loss of bowel or bladder control.
- Leg pain is accompanied by persistent weakness, tingling, or numbness in any part of the leg from the buttock to the ankle or foot.
- New low back pain is accompanied by vomiting and/or fever [101°F (38.5°C) or higher] that lasts longer than 48 hours.
- Leg pain or intermittent weakness, tingling, or numbness lasts longer than 1 week despite home treatment.
- You have back pain that either won’t go away or builds in intensity over a few weeks.
- A back injury is work-related, and symptoms don’t improve in 2 to 3 days.
- Back pain is accompanied by pain during urination or blood in the urine.
- You have back pain that is worse when you are resting than when you are active.
- You notice a gradual increase in problems with bowel or bladder control.
Watchful waiting
Watchful waiting is a wait-and-see approach. If you get better on your own, you won’t need treatment. If you get worse, you and your doctor will decide what to do next.
If you have pain, numbness, or tingling in one leg that gets worse with sitting, standing, or walking (without any obvious leg weakness):
- You may try a brief period of bed rest—usually no more than 1 to 2 days—then gradually begin activities if the pain is manageable.
- Take short walks.
- Avoid movements and positions that increase pain or numbness.
Who to see
For diagnosis and nonsurgical treatment of a herniated disc, you may see:
- A family medicine doctor.
- An internist.
- A chiropractor.
- A physical therapist.
- A physiatrist (a specialist in physical medicine and rehabilitation).
- A rheumatologist.
- A neurologist.
For diagnosis and surgical treatment of a herniated disc, specialists include:
- A neurosurgeon.
- An orthopedic surgeon.
Exams and Tests
Your doctor will do a medical history and physical exam. If this suggests that you have a herniated disc, you probably won’t need other tests.
If your doctor needs more information, or if treatment hasn’t worked after 6 weeks, you may have an MRI or a CT scan.
X-rays typically aren’t useful or needed. But if your medical history and physical exam suggest a more serious condition (such as a tumor, infection, fracture, or severe nerve damage), or if your leg pain and other symptoms don’t get better after 6 weeks of nonsurgical treatment, your doctor may order X-rays.
Other tests
Other tests, such as blood tests, may be done to rule out other conditions.
The following tests aren’t used as often as an MRI or a CT scan, but they may give your doctor more information:
- An electromyogram and nerve conduction test may be done in some cases for people who have signs of prolonged pressure on a nerve root.
- A myelogram may be done if you can’t have an MRI or if the results of an MRI aren’t clear.
- Discography can help diagnose disc problems but is rarely used.
- A nerve block may show which nerve is causing a problem.
Treatment Overview
Your doctor may recommend a short period of rest or reduced activity followed by a gradual increase in activity.
Usually a herniated disc heals on its own. So most of the time nonsurgical treatment is tried first, including:
- Heat or ice, exercise, and other steps at home to help with pain and make your back stronger. For more information, see Home Treatment.
- Physical therapy. For more information, see Other Treatment.
- Pain medicine. For more information, see Medications.
You’re likely to get the most benefit if you have treatment before you’ve had more than 6 months of symptoms.footnote 2
Surgery
Surgery can be a good choice for people who have nerve damage that is getting worse or pain that hasn’t improved after several weeks of nonsurgical treatment.footnote 1 For more information, see Surgery.
Prevention
To help prevent low back pain or a herniated disc:
- Stay at a healthy body weight. This may reduce the load on your lower back.
- Exercise regularly.
- Quit smoking. Nicotine can harm the discs in your back, because it lowers the ability of the discs to absorb the nutrients they need to stay healthy. And it may cause them to become dry and brittle.
- Useproper lifting techniques.
- Think about your posture. Slumping or slouching alone may not cause low back pain. But after the back has been strained or injured, bad posture can make pain worse.
- Use good posture while standing or walking. “Good posture” generally means that your ears, shoulders, and hips are in a straight line.
- Protect your back while sitting. Try putting a small pillow or rolled towel between your back and the chair.
- Keep your back in the neutral position while sleeping. Place a pillow between your knees when sleeping on your side.
Home Treatment
To reduce pain
The following steps may help to reduce pain:
- Relax. Find a comfortable position for rest. You might prefer lying on the floor or a medium-firm bed with a small pillow under your head and another under your knees. Or you can try lying on your side with a pillow between your knees. Don’t stay in one position for too long.
- Walk. Take a short walk (10 to 20 minutes) on a level surface (no slopes, hills, or stairs) every 2 to 3 hours. Walk only distances you can manage without pain, especially leg pain.
- Take pain medicine if needed. These medicines usually work best if you take them on a regular schedule instead of waiting until the pain gets worse.
- Try heat or ice. There is not strong evidence that either heat or ice will help, but you can try them to see if they help you. You may also want to try switching between heat and cold. You can try:
- A heating pad on a low or medium setting for 15 to 20 minutes every 2 to 3 hours.
- A warm shower in place of one session with the heating pad.
- Single-use heat wraps that last up to 8 hours.
- An ice pack for 10 to 15 minutes every 2 to 3 hours. You can use an ice pack or a bag of frozen vegetables wrapped in a thin towel.
To strengthen your back
Keep active and do exercises, as recommended by your doctor or physical therapist, to help you return to your usual level of activity. Core stabilization exercises can help you strengthen the muscles of your trunk to protect your back.
Medications
Although medicine doesn’t cure a herniated disc, it may reduce inflammation and pain and allow you to begin an exercise program that can strengthen your stomach and back muscles. Be safe with medicines. Read and follow all instructions on the label.
Medicine choices
- Pain relievers, such as acetaminophen (Tylenol, for example) and nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs include ibuprofen (such as Advil) and naproxen (such as Aleve).
- Muscle relaxants.
- Corticosteroids.
- Opioids.
- Antidepressants.
Surgery
Surgery is considered if the following conditions are present:
- You have leg pain that hasn’t improved with at least 6 weeks of nonsurgical treatment, and your symptoms are bad enough to interfere with normal activities and work and to require strong pain medicine.
- You have weakness, loss of motion, or abnormal sensitivity.
- Tests show that your herniated disc can be treated surgically.
People who have surgery may feel better faster. But in the long run, people treated with surgery and people treated without surgery have similar abilities to work and to be active.footnote 3 Some people require additional disc surgery after their first surgery.
Many people are able to gradually resume work and daily activities soon after surgery. In some cases, your doctor may recommend a rehabilitation program after surgery, which might include physical therapy and home exercises.
Disc surgery isn’t considered effective treatment for low back pain that is not caused by a herniated disc. Disc surgery is also not done if back pain is the only symptom the herniated disc causes.
Surgery choices
- Discectomy. This may be the most effective type of surgery for people who have tried nonsurgical treatment without success and who have severe, disabling leg pain.
- Percutaneous discectomy
- Laminotomy and laminectomy
Experimental procedures
A number of technologies using small incisions or injections for destroying the disc are used by some surgeons. Examples are endoscopic discectomy and electrothermal disc decompression. These techniques are experimental and unproved. If your doctor recommends one of them to treat your herniated disc, make sure to get as much information as possible about the procedure. Consider getting a second opinion.
Laser discectomy uses a focused beam of light to dissolve a herniated disc. Although this technology has been used by some surgeons for several years, it is considered experimental because of the lack of studies on its effectiveness and safety.footnote 4
Other treatments that have been tried include removing the center of the disc and removing all or part of the disc by using suction. These treatments are not considered to be effective.
Other Treatment
You can try other treatments besides medicine and surgery, including:
- Chronic pain management programs.
- Physical therapy.
- Rehabilitation programs.
Complementary medicine
Talk to your doctor before using complementary medicine to treat a herniated disc.
Some people use complementary medicine along with standard or conventional care to treat leg and back pain caused by a herniated disc. Some examples are:footnote 5
Related Information
References
Citations
- Tay BKB, et al. (2014). Disorders, diseases, and injuries of the spine. In HB Skinner, PJ McMahon, eds., Current Diagnosis and Treatment in Orthopedics, 5th ed., pp. 156–229. New York: McGraw-Hill.
- Rihn JA, et al. (2011). Duration of symptoms resulting from lumbar disc herniation: Effect on treatment outcomes. Journal of Bone and Joint Surgery, 93(20): 1906–1914.
- Atlas SJ, et al. (2005). Long-term outcomes of surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: 10-year results from the Maine Lumbar Spine Study. Spine, 30(8): 927–935.
- Jordan J, et al. (2011). Herniated lumbar disc, search date June 2010. Online version of BMJ Clinical Evidence: http://www.clinicalevidence.com.
- Jordan J, et al. (2011). Herniated lumbar disc, search date June 2010. Online version of BMJ Clinical Evidence: http://www.clinicalevidence.com.
Other Works Consulted
- Atlas SJ, et al. (2001). Surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: Five-year outcomes from the Maine Lumbar Spine Study. Spine, 26(10): 1179–1187.
- Deen GH, et al. (2003). Minimally invasive procedures for disorders of the lumbar spine. Mayo Clinical Procedures, 78: 1249–1256.
- Peul WC, et al. (2007). Surgical versus prolonged conservative treatment for sciatica. New England Journal of Medicine, 356(22): 2245–2256.
- Weinstein JN, et al. (2006). Surgical vs nonoperative treatment for lumbar disk herniation: The spine patient outcomes research trial (SPORT): A randomized trial. JAMA, 296(20): 2441–2450.
- Weinstein JN, et al. (2006). Surgical vs nonoperative treatment for lumbar disk herniation: The spine patient outcomes research trial (SPORT): Observational cohort. JAMA, 296(20): 2451–2459.
Credits
Current as ofJune 26, 2019
Author: Healthwise Staff
Medical Review: William H. Blahd Jr. MD, FACEP – Emergency Medicine
E. Gregory Thompson MD – Internal Medicine
Adam Husney MD – Family Medicine
Kathleen Romito MD – Family Medicine
Kenneth J. Koval MD – Orthopedic Surgery, Orthopedic Trauma
Current as of: June 26, 2019
Author: Healthwise Staff
Medical Review:William H. Blahd Jr. MD, FACEP – Emergency Medicine & E. Gregory Thompson MD – Internal Medicine & Adam Husney MD – Family Medicine & Kathleen Romito MD – Family Medicine & Kenneth J. Koval MD – Orthopedic Surgery, Orthopedic Trauma
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.